Case Study: Left Total Hip Replacement in a
77-year-old female with Hip Arthritis
A 77-year-old female presented with complaints of worsening left hip pain for the past year. She stated she worked as a hairdresser for the past 65 years and retired 2 years ago. She noticed the pain while prolonged standing which was insidious and without any precipitating injury.
The pain was described as a sharp pain located in the left groin which varied in intensity from moderate to severe (6/10). The pain was constant and especially worse while navigating stairs, prolonged standing, getting up from chair, bending and squatting. Her walking tolerance was limited to only 2 blocks secondary to groin pain. She was using a cane as an assistive device. Occasionally the pain would radiate down to the left thigh and buttock.
She was living with her husband and expressed anguish at her inability to perform daily activities due to pain. She stated, her sleep was disturbed due to pain and she would have daytime sleepiness. She was unable to stand to cook food or go to a nearby deli. She was apprehensive about traveling because of prolonged sitting.
She was a nonsmoker and nondrinker. Her medical history included hypertension, dyslipidemia, and asthma. All her medical conditions were well controlled with medications. Her surgical history included resection for rectal cancer and uterine fibroidectomy done fifteen years ago. She denied any known drug allergies.
The patient tried conservative management in the form of physical therapy. She also had a hip injection 6 months ago with minimal relief. She had also tried NSAIDs but the relief was only temporary. Recently, she heard about hip arthroplasty and wanted to explore the option for possible hip replacement.
On physical examination, her gait was antalgic with no lurch. The stance phase of the gait was reduced on the left side. There was no exaggerated lumbar lordosis or scoliosis. Both the anterior and posterior iliac spines, patella, and medial malleolus were at the same level.
On the supine examination, there was no leg length discrepancy. The skin overlying the left groin was normal, there were no scar marks or sinus tracts. There was no fullness in the Scarpa’s triangle and no enlarged inguinal lymph nodes. There was no local rise of temperature and no tenderness of the greater trochanter. There was mild tenderness of the left anterior groin.
The range of motion was moderately restricted, especially in internal rotation and extension. The bulk and tone of the muscles were normal. The straight leg test was positive with pain in the groin. There was no fixed deformity of the left hip. The distal neurological examination of the bilateral lower extremities was normal.
The examination of the contralateral hip, bilateral knees and ankles were normal. The deep and superficial tendon reflexes were present and symmetrical. There was no bowel bladder abnormality. The bilateral lower extremity pulses were good volume and comparable.
Imaging revealed osteoarthritic changes of the left hip joint with joint space reduction, subchondral cyst, sclerosis, and osteophyte. Having exhausted conservative management options, the patient was advised left total hip replacement. Risks, benefits, and alternatives were discussed with the patient at length. She agreed to go ahead with the procedure.

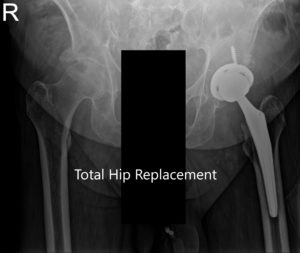
Preoperative X-ray showing the Judet view of the pelvis.


Preoperative X-ray showing the frog-legged lateral and AP view of the left hip.
OPERATION: Left Total Hip Arthroplasty.
IMPLANT USED: Acetabulum shell 54-mm with 0-degree polyethylene insert, 36-mm inner diameter with a femoral head, 36 mm plus 5 with a 6.5 mm x 30 mm screw.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining an informed consent and signing the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient prior to the procedure.
The patient was brought to the operating room where anesthesia was obtained by the anesthesiologist. The patient was then definitively positioned with the left hip up, and the left hip was then draped and prepped in the usual sterile manner.
The skin incision was made centered over the greater trochanter, and the skin and subcutaneous tissues were then incised. The fascia was then divided. The hip was then placed in internal rotation, and the posterior soft tissue structures were then taken down and tagged for future repair.
The hip was then dislocated. Lesser trochanter to the center measurement was taken, and neck resection was then made. The head was then removed. Attention was then turned towards the acetabulum. The remainder of the labrum was then debrided, and acetabulum was then sequentially reamed.
The final shell was then placed into position in the correct abduction and anteversion after removing the cyst and grafting the defects. An additional screw was used for
fixation. The poly was then placed over the shell. The anteversion and abduction were confirmed.
Attention was then turned towards the femur. The remainder of the tissue on the undersurface of the greater trochanter was then removed. The femur was then sequentially broached. The final broach was left into position. The trunnion and the head were then placed over the broach.
The lesser trochanter to center measurement was taken, and the additional length was built for compensating for the shortening. The hip was then trialed for the trial range of motion and was found to be stable. The trial components were then removed. The final components were then placed into position.
Thorough irrigation was performed. Drill holes were made in the greater trochanter, and the posterior soft tissue structures were then tacked to the greater trochanter through transverse tunnels. Thorough lavage was given. Fascia was. closed with Ethibond.
Cutaneous tissues were closed with 2-0 Vicryl, the skin was closed in layers. Sterile dressing was applied over the wound, and the patient was then transferred to the postoperative care unit in stable condition.
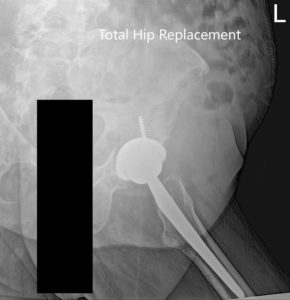
Postoperative X-ray of the Pelvis and lateral view of the left hip.
The recovery of the patient was expedited with management of pain with medications. Post-op there was no leg length discrepancy and no distal neurovascular deficit. Her vitals remained stable and weight-bearing was allowed as tolerated with support.
Rehabilitation was started with a focus on gait and transfer training, fall prevention, and physical therapy. Aspirin was continued for 6 weeks and pain medications were taped off. She was compliant with hip precautions and continued abduction pillow at night. Three months post-op she demonstrated full pain free range of motion. She was able to walk without support and was happily back to the activities she enjoyed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.

