Case Study: Revision Total Hip Replacement in a 64year old. Isolated acetabular component exchange
A 64 year-old female who previously had a Total Hip Replacement over a decade ago. She initially did well following her recovery and remained symptom-free up until several years ago she started to notice to some soreness in her hip that was new. It gradually worsened over time despite her attempts to alleviate it with physiotherapy and medication.
She presented to our clinic with new X-rays that demonstrated asymmetric polyethylene wear in her acetabular component liner. Acquisition of the details of her implants revealed that she did receive an older-generation polyethylene liner, which is known to exhibit signs of wear towards the end of its lifespan.
She is otherwise healthy with no major contributory medical or surgical issues, no known drug allergies and regular medications only for anxiety and hypothyroidism. She has been fit and active up until the onset of her new hip pain.
More detailed examination of her radiographs revealed signs of bone loss around the acetabulum, likely as a result of an inflammatory response generated by polyethylene particles generated from the wear phenomenon. Her femoral component appeared intact with no major issues.
We counselled Mrs. IS that she would require revision surgery of her acetabular component due to her polyethylene wear, and that we would need to revise her entire acetabular component as the type of liner she had implanted is no longer made, but also due to the possibility of loosening of her acetabular component as a result of the bone loss from the polyethylene wear.
She accepted and consented, and we planned for her to receive surgery as soon as possible. We performed a posterior approach – the approach used for her first hip replacement and exposed her artificial hip fully. We dislocated it and used special instruments to first remove her acetabular liner, and then her acetabular component. We observed minimal bone loss, and so placed a slightly larger revision acetabular component in its place, ensuring stability and leg length were both restored.
Mrs. IS recovered within 3 months of her surgery, and is back to being fit and active and pain-free in her right hip.
Pre-op
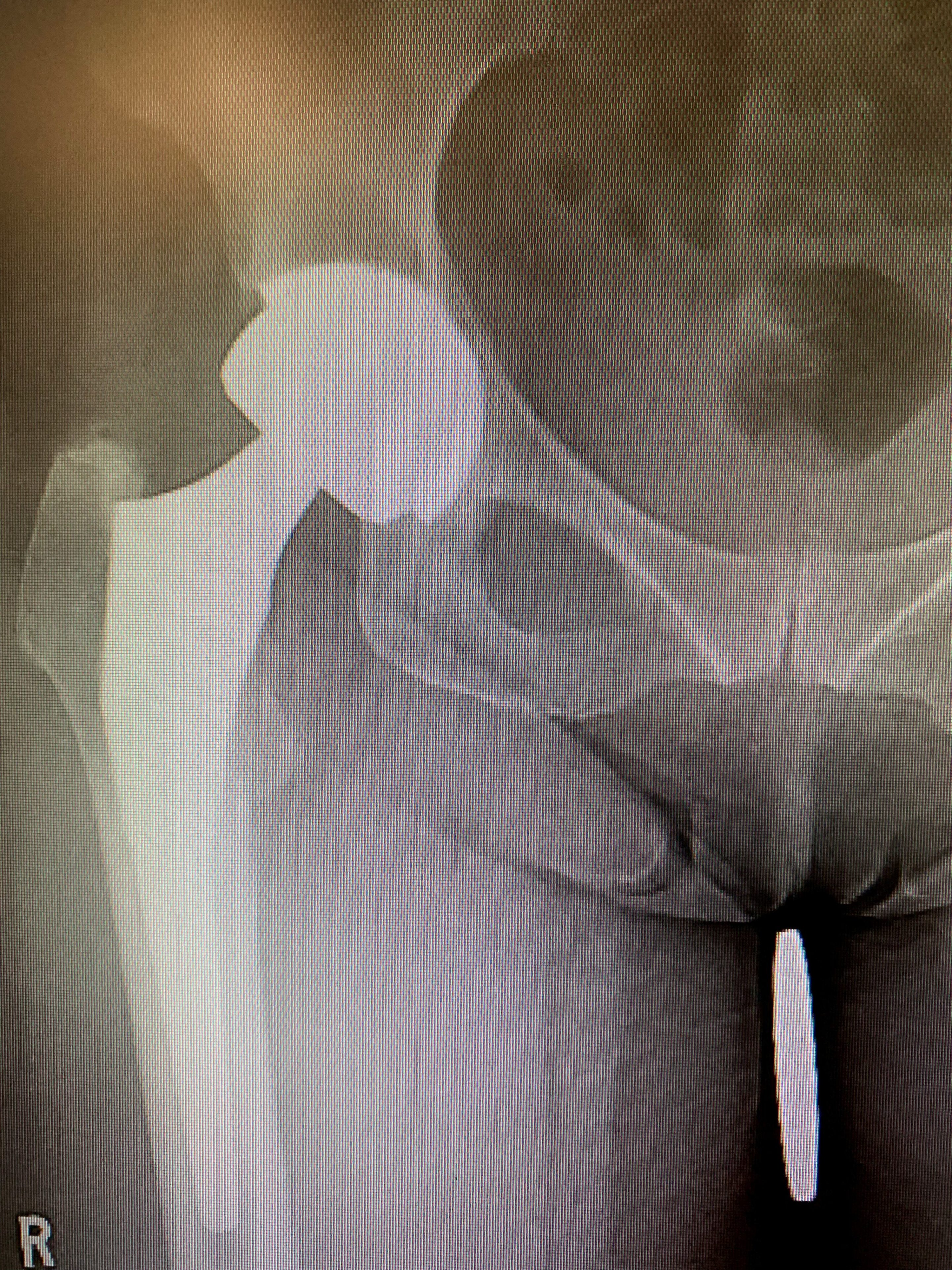
Revision total hip replacement in a 64-year-old. Isolated acetabular component exchange.
Post-op
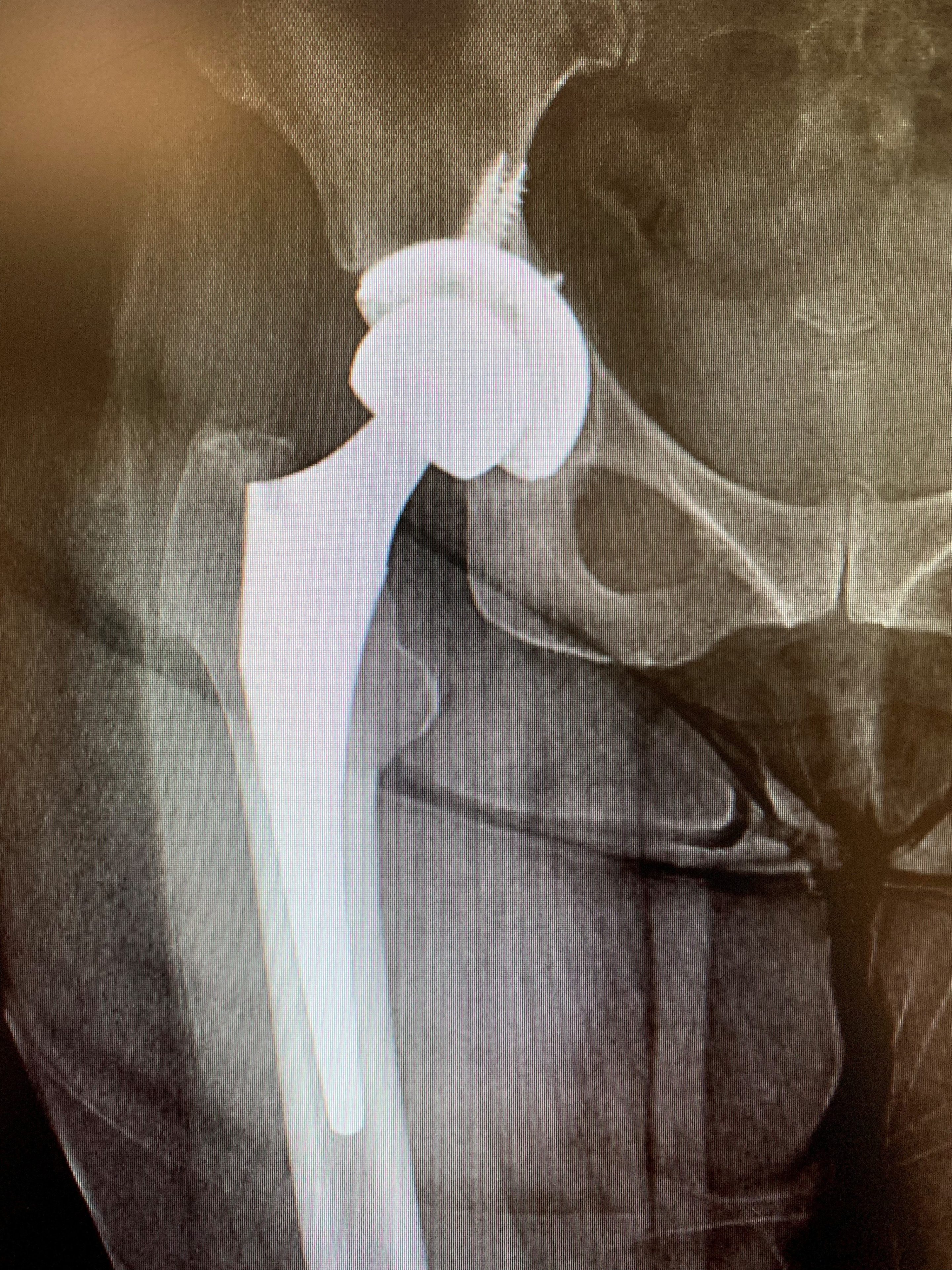
Revision total hip replacement in a 64-year-old. Isolated acetabular component exchange.
