Case Study: ACL, Arthroscopic Assisted Reconstruction
with Autograft in a 38 year-old guy
Arthroscopic surgery is used to repair the ACL, which is less intrusive and allows patients to recover faster. The injured ligament is restored in an ACL reconstruction with a tissue graft from a donor (allograft) or your own body (autograft).
The patient is a 38-year-old guy who came into the office complaining of discomfort and instability in his right knee. He added that he had previously seen a doctor who diagnosed him with an ACL tear. A knee MRI was done which confirmed the absence of ACL. Physical examination was positive for ACL deficiency.
We talked about treatment with the patient. The patient had already tried physical therapy. We discussed treatment alternatives, and the patient was advised to have surgery. We addressed the dangers and benefits, which included infection, hemorrhage, nerve and vascular injury, operation failure and the need for repeat surgery, and arthritis, among other things.
We talked about systemic issues including blood clots, cardiac or pulmonary difficulties, and so forth. The patient was aware of the situation and granted informed permission.
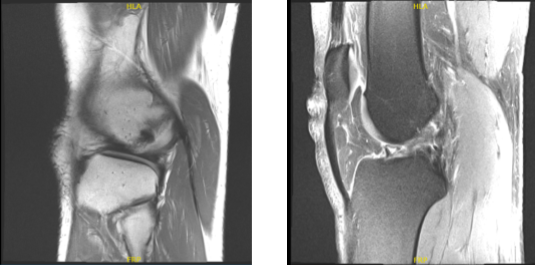
MRI right knee non-contrast
The patient was brought to the surgery room and placed on a comfortable operating table. The anesthesia department administered a local block. The patient was put under general anesthesia and intubated.
Following tourniquet administration, the right lower extremity was prepped and draped aseptically in the usual manner. Antibiotics were administered before surgery. A timeout was issued. After Esmarch, the tourniquet was raised. Anesthesia examination revealed a gentle termination.
An incision was made into the quadriceps from the proximal pole of the patella. An incision of around 2 cm was created. The quadriceps region was freed after thorough dissection. The paratenon was severed along the incision line.
The paratenon was severed proximally from the quadratus tendon and distally from the patella. The tendon was visible during retraction. A linear flap was discovered on the skin for severing the quadriceps tendon. 10 mL was used to cut a 10 mm quadriceps tendon from the tip of the superior pole of the patella into the quadriceps tendon just lateral to the vastus medialis.
The quadriceps tendon was raised from the proximal volar patella using a knife. Sharp dissection was used to raise a full thickness quadriceps bone transplant. The cigar cutter was then inserted to withdraw the graft.
A 68 mm section of quadriceps tendon was cut and placed on the back table. The knee joint capsule was not reached during the procedure. Brian Jones, PA, on the back table, prepared the quadriceps tendon with FiberLink on both sides and tight ropes.
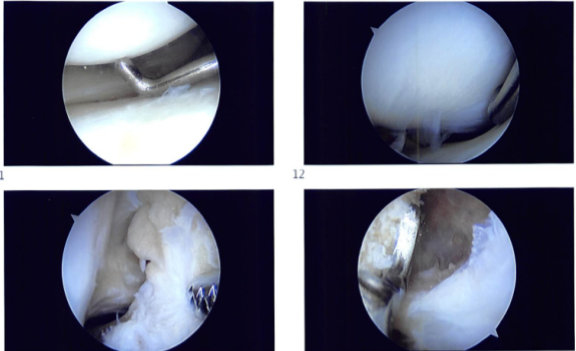
The arthroscope was inserted through a lateral anterior portal created by a lateral parapatellar incision. The patellofemoral compartment was found to have complete cartilage. The meniscus and cartilage in the medial patellofemoral compartment were found to be intact.
The anterior condyle notch was examined and found to be devoid of ACL from the proximal connection. The lateral tibiofemoral compartment was examined and found to have intact cartilage with degenerative tearing and across the margin of the lateral meniscus with no debridement because the meniscus was intact.
To remove the ACL stump and prepare the medial surface of the lateral femoral condyle at the intercondylar region for the bone graft, the intercondylar notch was debrided. In the preparation phase, a shaver and a coblation wand were employed.
The quadriceps tendon was repaired, resulting in a 9.5 mm quadriceps graft. Fiber Links were used on both sides. Measurements were taken, and it was determined that it was 35 mm on each side. The ACL femoral was now implanted on the medial surface of the lateral femoral compartment, medial femoral condyle, via the lateral portal.
An incision was created over the lateral femoral condyle, and the sleeve was inserted with the zig at 10:30, about 7 mm from the posterior condylar border. The sleeve was pressed to the bone, and then a flip cutter was inserted.
The flip cutter was inserted via the medial surface of the lateral femoral condyle. When the sleeve was in the proper place, it was impacted into the bone, the flip cutter was flipped to 9.5 mm, and a 30 mm tendon was split into the femoral condyle.
The flip cutter was put back into the knee joint and closed, followed by the insertion of a fiber loop, which was removed and logged onto itself. The arthroscope was now placed through the lateral anterior portal, and the tibial tunnel was prepared.
A 10 mm tibial lig was introduced posterior to the intermeniscal ligament and placed just medial to the medial tibia. A secondary skin incision was made before inserting a sleeve. A flip cutter was inserted and drilled once more to create a tibial tunnel.
When the sleeve was in the proper place, it was hit again onto the bone, and the flip cutter was flipped to 9.5 mm, creating a 30 mm tunnel. The flip cutter was removed, and the tibial tunnel was capped with Fiber Loop that was fastened onto itself.
The Fiber Loops were extracted from the lateral portals, and the medial portal site was suitably patched for tendon passage. The tibial loop was now opened, and the graft was put onto the femoral loop and implanted through the lateral portal with the arthroscope.
Sutures were visible passing, followed by the button being flipped on the lateral femoral cortex. The term was now employed to draw the tendon in. Approximately 25 mm of tendon was dragged into the tunnel. At this point, the graft side was put onto the tibial fiber loop and traveled into the tibial tunnel, with roughly 20 mm of graft passing on the tibial side.
The button was again flipped onto the tibial cortex and toggled to tighten the graft. The graft was discovered to be in the proper place. The knee cycled thirty times, and the tight ropes were tightened on both sides.
The graft was examined and there was no evidence of impingement. Sutures were placed beneath the skin. After extensively irrigating the knee, the final photographs were stored. The wounds were closed with 2-0 Vicryl and 3-0 Monocryl. Dressing was done using Adaptic and Dermabond, Steri-Strips, 4 x 4, ABD, Webril, and ACE wrap. A knee immobilizer was worn. In stable condition, the patient was extubated and brought to the recovery room.
Introperative images
After one week the patient was seen in the office for his postoperative visit, no x-rays were needed. His pain is well controlled and he denies fever or chills. We opted to proceed with official physical therapy as well as a home workout regimen for knee rehabilitation after examining treatment choices.
During the visit, we removed the stitches. We will continue to use ice and elevate the knee to reduce swelling and pain. To limit the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis.
We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications. We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
After one month the patient went to the office for his post operative consultation, no x-rays were needed. His pain is well controlled and denies fever, chills. He was taken to LICH, Brookhaven and was discharged.
His knee is worse and the back still hurts. No PT started and we discussed treatment options including PT, MRI, Injection, surgery. We agreed to go with conservative management for now.
After three months the patient is here today for his postoperative visit, he is now able to walk without a brace and is improving and PT to be started as discussed.
With ongoing physical therapy and rehabilitation for the knee, the patient responded well following surgery and is steadily getting better each time he is seen. The patient recovered and healed with continued physical treatment and regular visits.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.