Case Study: Medial Patellofemoral Ligament (MPFL)
Reconstruction, Lateral meniscectomy and Chondroplasty of the Left Knee
A 36-year-old male patient is in our office, with complaints of left knee pain for the past 2 months. The patient had gone to the ER 2 months ago, to place kneecap back into the socket. The patient stated leaving the ER, there was no more pain. The patient states he used to pop his kneecap back into place, by himself.
The patient describes the knee pain as sharp, dull, stabbing, throbbing. The pain is associated with swelling, bruising, numbness, tingling, and radiating pain. The pain is not associated with weakness, bowel or bladder abnormality, gait problem, giving way, or limping.
The patient states that the problem has been getting better since it started. Activities involving bending the knee make the symptoms worse. Knee mobilizer makes the symptoms better. The patient has undergone surgery for the left knee, carpal tunnel, and c-section. The patient has no medical history. The patient has no allergies. The patient is currently taking no medication. The patient does not smoke.
The patient has previously tried icing, physical therapy and over the counter pain medication without significant relief. He works for cleaning services and is not able to work without considerable pain at present.
On general physical examination the patient was calm conscious cooperative and well oriented to time place and person. The gait of the patient is antalgic walking without support. Upon examination of the left knee, the patient is nontender to palpation along the medial and lateral joint lines and has mild effusion.
There is tenderness on palpation along the medial aspect of the patella and medial patellofemoral ligament. They have no crepitus of the patellofemoral joint with the range of motion but the patient is apprehensive about patella glide testing.
The patient has no discomfort with McMurray’s s maneuvers, and the knee is stable. The range of motion of the knee is limited. There is 5/5 strength in bilateral lower extremities with no distal neurovascular deficit. There are no erythema, warmth, or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has an excellent range of motion, stability, and strength.
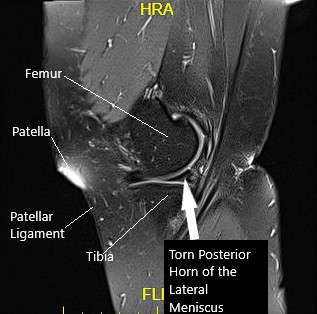
Sagittal MRI image of the left knee
MRI suggested lateral meniscus tear and trace joint effusion with possible recurrent patellar instability. We discussed treatment options and opted for surgical management. We discussed risks and benefits as well as complications including infection, bleeding, repeat surgery, injury to adjacent nerves. The patient agreed to go ahead with the procedure.
PREOPERATIVE DIAGNOSES:
- Meniscus tear, left knee.
- Recurrent dislocation of the patella left knee.
POSTOPERATIVE DIAGNOSES:
- Lateral meniscus tear, left knee.
- Instability of patella, left knee.
OPERATION:
- Left knee arthroscopic lateral meniscectomy.
- Left knee arthroscopic chondroplasty of the patella and the medial femoral condyle.
- MPFL reconstruction using gracilis allograft and biocomposite 4.75 SwiveLock x2 in the patella, 6.0 mm biocomposite interference screw in the femur.
PROCEDURE: The patient was taken to the operating room area where she was put on a well-padded operating table. General anesthesia was induced. Left lower extremity was prepped and draped aseptically. A preoperative antibiotic was given. Time-out was done.
A lateral entry portal was made for the arthroscopic examination. The arthroscope was inserted. There was a small patch of grade 2 to grade 3 arthritis on the medial patellar area, which was cleaned by shaving. The examination of the intercondylar notch was intact native ACL.
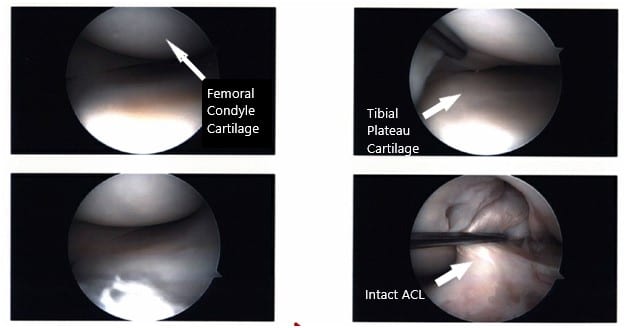
Intraoperative Arthroscopic images of the left knee.
Examination of the tibiofemoral joint showed a tear of the medial margin of lateral meniscus, which was cleaned using a shaver and up biters. There was no tear in the medial meniscus. There was large popliteal hiatus with the possible tear going into the posterior horn of the lateral meniscus, which was incomplete.
A thorough examination was done and the debridement was done. The decision was done not to repair it at present because it seemed to be an extension of the popliteal hiatus.
Now the scope was removed and a medial incision was given over the superior medial margin of the patella. Tendon was exposed and the medial margin of patella cleaned and decorticated. Two guidewires were passed under C-arm. Reaming was done over the guidewire. In the meantime, the graft was prepared on the back table.
Another guidewire was passed in the patella about 15 mm distal. Reaming was also performed. The free end of the tendon was inserted into the patella on the superior and inferior holes using SwiveLock. Now the femoral point was found using an MPFL guide and incision was given after checking under C-arm. The dissection was reached to the medial femoral condyle.
A guidewire was placed again and checked under C-arm and found to be in an appropriate position. It was put into the femoral and from medial inferior to posterior superior direction. The dissection was done between the second and third layers of the medial knee at the patella and tonsil clamp was used and passed onto the femoral site.
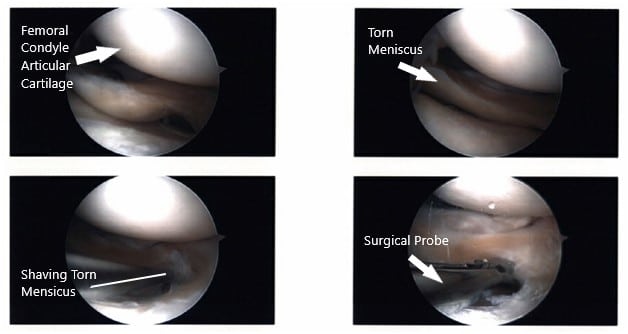
Intraoperative Arthroscopic images of the left knee.
The suture was passed back from there and the tendon was passed back into the femoral site and delivered. It was tied around the wire and found to be in an acceptable position which was tied in 30-degree flexion and loosened in 90 degrees of flexion as well as extension.
The Beath pin was passed through and through. Reaming was performed for 40 mm over the Beath pin. The sutures through the tendon loop were passed through the Beath pin and passed out laterally. An appropriate tension not to over tighten the patella was put with 30 degrees of flexion and excision of the tendon was done with an interference screw.
The final tendon was checked and found to be satisfactory. The sutures were removed and the patella sutures were used for reinforcement and cut. Closure of the wound was done after irrigation in layers. Monocryl was used for closure. The dressing was done using 4 x 4, ABD, Webril, and Ace wrap. Bledsoe brace was applied and was put in extension.
The patient was extubated. The femoral canal block was done by the anesthesia for pain relief. The patient was informed preop about that as well as optimal injury to her mother about the precautions as well as the use of a brace. The patient was asked to use the medication, ice, and elevation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
