Case Study: Knee Arthroscopy: Lateral Meniscectomy
Lateral Femoral Condyle and Trochlear Chondroplasty
in a 44 year-old patient
An arthroscope, and surgical instruments were inserted into your knee through a series of tiny incisions by your doctor. For many days, you’ll feel worn out. You’ll get swelling in your knee. Additionally, you could observe that the area around the cuts (incisions) has a distinct tone of skin.
The shinbone (tibia) is covered in thick, springy bands of cartilage called the medial and lateral meniscectomy. They stabilize the knee and serve as shock absorbers. Size and severity of meniscus tears can vary significantly.
The most frequent knee injuries include sprains, rips, dislocations, and fractures. Some of the most frequent sports injuries affecting the knee are meniscus tears and tears of the anterior cruciate ligament (ACL). Although less frequent in sports, patella (kneecap) fractures can occur from high-impact trauma.
Repairing damaged knee cartilage with a chondroplasty is a minimally invasive surgical treatment. A surgeon uses arthroscopic technology to remove damaged joint tissue and assist in addressing any potential issues in the future. Healthy cartilage can develop where diseased tissue once did by being removed.
A 44 year-old patient was in our office, she had hyperextended left knee and had trouble walking, it still is not better. Can walk but can’t kneel or run w/o shooting pain. She has tried NSAIDs and exercises.
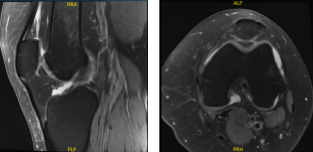
She was in the office with MRI results that showed complex multidirectional tear free edge lateral meniscus on the background of mild lateral compartment osteoarthritis. Mild patellofemoral compartment osteoarthritis as well.
MRI-3 Left knee non-contrast
We discussed treatment options and options for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, arthritis, rehabilitation, need for total knee replacement, and diffuse surgery in future.
We also discussed systemic complications including blood clot, cardiac, pulmonary, neurologic complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. A low thigh tourniquet was applied on the left thigh. The thigh was put in a C-clamp. Esmarch was applied and tourniquet was elevated to 300 mmHg.
The left knee was prepped and draped aseptically in the usual fashion. Antibiotics were already given. Lateral entry portal was made and an arthroscope was inserted. A spinal needle was inserted from the medial side to become a medial portal which was accessed to the lateral compartment.
Shaver was introduced. Examination of the medial tibial femoral component showed intact meniscus and cartilage. Examination of the intercondylar notch showed intact ACL. Examination of the patellofemoral compartment showed intact patellar cartilage, but there was osteochondral lesion of the trochlea from grade 3 to grade 4.
Examination of the lateral tibiofemoral compartment showed tear of the posterior horn and body of the lateral meniscus along with grade 3 to grade 4 osteochondral lesion. Debridement of the meniscus as well as the cartilage was done with the use of biters and shavers. Balanced edges could be achieved.
The lateral femoral compartment osteochondral lesion measured about 1 cm x 3 cm. Trochlear lesion was also measuring about 1 cm x 4 cm. All balanced margins could be achieved.
The arthroscope was removed and the knee was thoroughly irrigated and drained. Closure was done with the use of # 3-0 nylon. Then, 20 cc of Naropin 0.5% mixed with 40 mg of Depo-Medrol was injected. Dressing was done with the use of Xeroform, 4 x 8, ABD, Webril, Ace wrap. The patient was extubated and moved to the recovery unit in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.