Case Study: Right Knee Arthroscopic: Medial
Meniscectomy and Plica Excision in a 63 year-old patient
An arthroscopic procedure called a plica resection involves removing aberrant synovial tissue from the knee joint. Plica, which are organic folds in the synovium of the knee joint, may frequently become uncomfortable and inflammatory.
Bone and cartilage in the joints may deteriorate. Damage to the nerves, muscles, or ligaments. A broken bone may rip or harm nearby soft tissues. clots of blood.
A 63-year-old patient was in our office with complaints regarding pain in his knees which was severe, and he felt that something was broken. He described the pain as sharp. He stated that his right hand and lumbar spine are mild in nature. T
he biggest problem is his knees he feels clicking and popping. He had some arthritis in the right knee before the accident, but it was all right after a steroid injection. The pain in the right knee is worsened, severe and different from the one before.
He presented X Ray of his bilateral knees, lumbar spine, and right hand from Zwanger. His Xray results showed mild osteoarthritic degenerative changes. There are no fractures. For his lumbar spine mild multilevel lumbar degenerative changes. For his right hand, normal right hand.

Left and Right knee X-ray complete with patella

LS Spine X-ray Flex/Ext no obliques

Right hand X-ray complete 3 or more views
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery. The patient expressed understanding of these risks and has elected to proceed with surgery.
I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
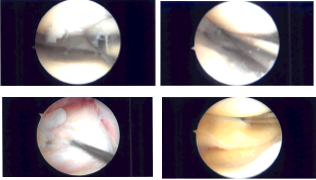
The patient was brought to the operating room where general anesthesia was induced. The right knee was prepped and draped aseptically in the usual fashion. Preoperative antibiotic was given. Lateral entry portal was made. Lateral parapatellar incision was made. Arthroscope was inserted.
The arthroscope was moved to the medial tibial femoral compartment where a medial entry portal was made with the use of a spinal needle. Examination of the medial tibiofemoral compartment showed radial tear along the body of the medial meniscus with ragged margins.
There was grade 1 to grade 2 osteoarthritic changes of the medial femoral condyle, which was cleaned with a shaver. The tear was not amenable to any repair. So, partial meniscectomy was performed with the use of right-sided biters, straight biter as well as shaver. Balanced margins were achieved.
Examination of the intercondylar notch showed intact, ACL with some degeneration. Examination of the lateral tibiofemoral compartment showed intact cartilage as well as meniscus. There was grade 1 to grade 2 osteoarthritic changes of the lateral femoral condyle in the region of trochlea, which was cleaned with the use of shaver.
Examination of the patellofemoral compartment showed intact Cartlidge. There was a inflamed suprapatellar plica extending from medial to lateral capsular wall. It was excised using the use of shaver. Final pictures were taken and saved.
The knee was thoroughly irrigated and drained. Closure was done with the use of 3-0 nylon. dressing was done with The use of Xeroform, 4 x 4, ABD, webril, ace wrap. Patient was extubated and moved to recovery in stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
