Case Study: Left Total Hip Replacement in a 55-year-old
male with Avascular Necrosis (AVN) of the Left Hip
A 55-year-old male patient presented to our office with complaints of left hip pain associated with stiffness. The pain was first noticed three years ago and gradually progressed over time. The patients had a history of left hip dislocation managed with closed reduction outside the United States five years ago.
The patient was apparently well five years ago when he sustained a fall from height while working on a roof. He sustained a left hip dislocation as a result of the fall. He was managed at a hospital with a closed reduction of the leg hip joint. The patient recovered well and didn’t experience any pain. Two years later he started experiencing mild discomfort in the left groin.
The discomfort was described as a dull ache which was constant. The intensity gradually increased to moderate in intensity and recently disturbed his sleep at night. He was told that he had avascular necrosis of the left hip. Medications were prescribed from which the patient received a minimal benefit.
He was employed by a construction company currently out of work due to pain. He used a cane as an assistive device. The pain was worse with activities such as walking, going up and down the stairs, bending, squatting and getting up from a chair. He was able to walk only two blocks without any discomfort. He had earlier tried pain medications but the relief was only temporary.
He was an occasional cigar smoker and consumed alcohol in moderation. The patient had no history of any significant medical illness. His surgical history was positive for left forearm open reduction and internal fixation when he was twenty years old.
On his physical examination, he walked with an antalgic gait with a reduced stance phase on the left side. The bilateral shoulders, iliac spines, and the patella were at the same level. There was no evidence of exaggerated lumbar lordosis. The spine examination was negative for any functional or structural scoliosis.
There was no evidence of scar marks or sinus tracts on the left groin. There was no erythema and no local rise in temperature. There was an absence of any swelling and inguinal lymphadenopathy. Tenderness was present on the left anterior joint line.
The bilateral anterior superior iliac spines were at the same level. There was no leg length discrepancy. The range of motion was moderately restricted in the abduction. The rotational movements were painful. There was no evidence of any fixed deformity. There was a differential rotation on left hip flexion.
The examination of the right hip, bilateral knee and ankles were normal. The power sensory examination of the lower extremities was unremarkable. The bilateral lower extremity tendon reflexes were present and comparable. The distal peripheral pulses were palpable and comparable.
Imaging studies obtained in the form of an X-Ray suggested sclerosis of the left head of the femur. There were marked acetabulum changes. An MRI was further obtained suggesting avascular necrosis of the superior lateral head of the femur with changes in the acetabulum. There was marked hypointense areas on both T1WI and T2WIs.
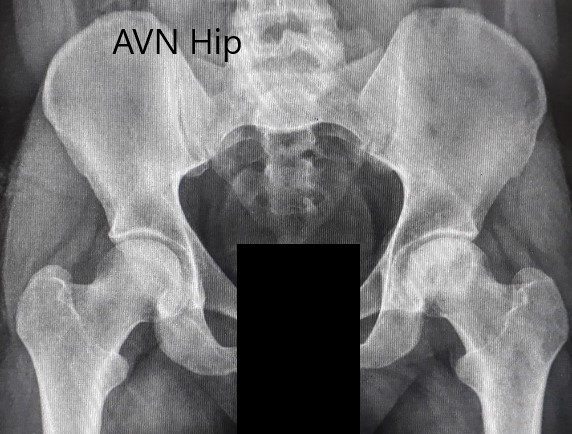
Preoperative X-ray of the pelvis with both hips in anteroposterior view showing AVN of the Left Hip.
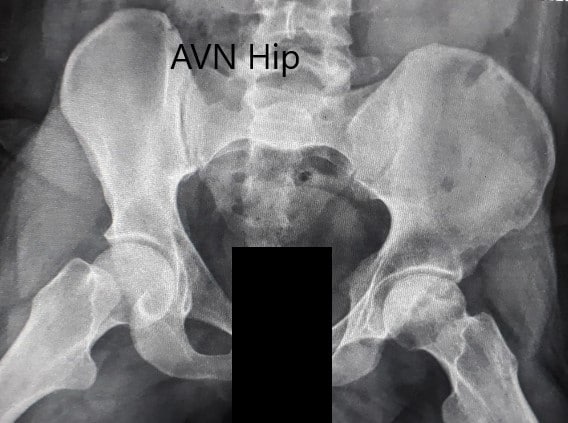
Preoperative X-ray of the pelvis with both hips in the frog-legged lateral view showing AVN of the Left Hip.
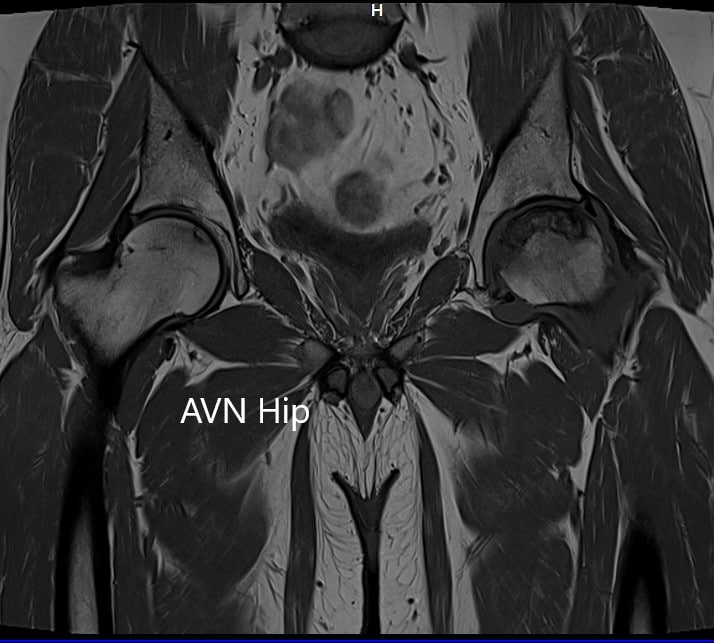
T1WI coronal section of MRI showing AVN hip.
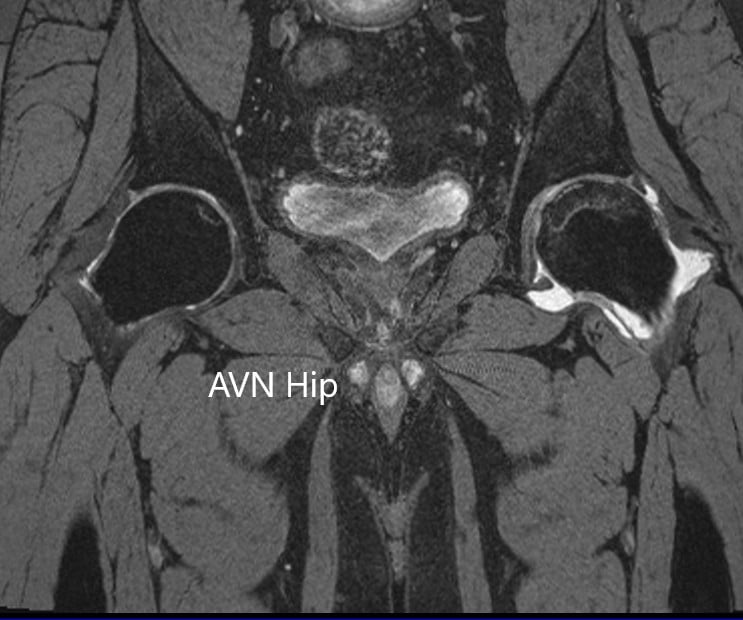
T2WI coronal section of MRI showing AVN hip.
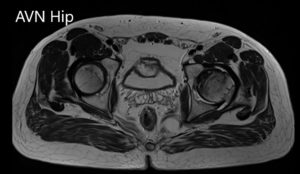
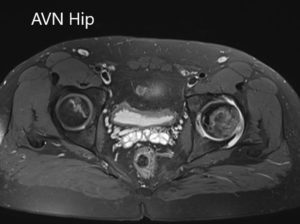
Axial sections of the T1WI and T2WI of MRI.
After careful consideration of the patient’s condition, he was advised left total hip replacement. The patient was made aware of the risks, benefits and potential complications of the procedure. The patient agreed with the plan and went ahead with the procedure.
Postoperative pain was managed with medications, he was prescribed aspirin for deep vein thrombosis prophylaxis. Weight-bearing was allowed as tolerated. The sutures were removed 14th-day post-op and the wound was dry, clean and intact.
Three months following the procedure, he was driving his car, walking without the support and gradually weaned off the hip precautions. He had successfully completed physical therapy and had a full range of motion. The patient was back to his baseline and had joined a new job at a supermarket. He was overjoyed with the success of the procedure and the relief of pain.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
