Avascular Necrosis of the Hip Joint
Bones in our body are living tissues which require a blood supply to nourish and keep them healthy.
Avascular necrosis of the hip is a condition resulting from the disruption of vital blood supply. No blood supply(avascular) leads to bone death called necrosis.
The condition is also known as osteonecrosis, aseptic necrosis or ischaemic necrosis, and here at Complete Orthopedics, we are specialists in treating Avascular Necrosis.
I’m Dr. Nakul Karkare, and I hope you’ll take a minute to watch this video…
Anatomy of the Hip Joint
The hip joint is a large weight bearing ball and socket joint. The ball is formed by the upper part of the thigh bone (femur) which fits into a socket formed by the acetabulum, which is part of the large pelvic bone.
The ball and the socket are covered by a smooth glistening white tissue known as cartilage. It helps in the smooth gliding of the ball in various movements about the joint such as walking, running,squatting, sitting cross legged.
Our own Dr. Karkare was on a recent WCBS 12 segment about Avascular Necrosis with Dr. Max Gomez:
Stages of Avascular Necrosis
Blood supply is vital to maintain the normal surface and structure of the joint. Any cause leading to decreased or absent blood supply leads to small islands of dead bone. Normally any area of dead bone is removed by the body and new bone is laid down to replace it.

X-ray showing avascular necrosis (AVN) of the hip
With an absent blood supply, a segment of bone is necrosed.
The surrounding bone with blood supply tries to revascularize the dead bone.
Vascular tissue lays down new bone in the area which increases the density (visible as increased whiteness in an X ray.)
A small fracture or break develops between the new bone and the dead bone.
The space in between the break is filled by a scar tissue.
Overlying cartilage without nourishment softens and decays. The weight bore on the joint leads to small dents or breaks in the cartilage leading to collapse.
The smooth gliding is now lost and the ball grinds with the socket in the area. The process becomes widespread leading to severe arthritis and destruction of the joint surface.
Causes & People at Risk
- Trauma: Injuries including fractures and dislocations(such as ball coming out of the socket) of the hip joint can compromise the vital blood supply leading to avascular necrosis. Any age group can be involved and the disease process is limited to the joint affected by trauma
- Alcoholism : Alcohol intake over the years causes direct toxicity to the bone cells and their blood supply. Certain drugs are also toxic to the bone cells. The result is areas of dead bone with collapse of the cartilage.
- Steroid abuse : Long term steroid use causes blockage to the blood supply in the hip. The reasons are unknown but one hypothesis is that increased fat globules in the blood which get lodged in the vessels. Commonly affecting patients on long term steroid therapy(transplant patients, kidney disease etc) and bodybuilders/athletes abusing steroids.
- Blood disorders : Patients with diseases causing thickening of blood are at risk due to increased chances of blood clot lodging in the vessels.
- Chronic liver disease : Hyperlipidemia or increased lipids in the blood cause fat globules to lodge and block the blood supply
- Others : Certain congenital(born with) diseases like Gauchers, sickle cell disease are at risk. Deep sea divers develop divers disease or the bends which makes them prone to develop avascular necrosis
- Unknown : Certain people develop it without any obvious cause most commonly affecting men in the 30’s to the 50’s of life. Eventually the other hip gets involved in 75% of the patients. When occurring in young adults or in the 20’s the disease is known as osteochondritis dissecans
- Surgeries around the hip : Often surgeries which are done to fix hip fractures, hip dislocations or to correct birth defects in the hip joint lead to damage to the blood supply.
Symptoms
- Hip Pain & stiffness: The starting complaints are usually mild to moderate pain in the groin or buttocks which may seem to go down to the thigh or even the knee. Stiffness around the hip develops and is associated with increased pain as the patient tries to move.
- Limp : Patient tries not to bear weight on the affected limb owing to increased pain and stiffness. As a result the patient walks with a limp which is usually noticed by the patient’s family or friends.
- Restriction of movements : Certain movements such as one required to tie shoelaces may be the first to be limited. With advanced disease all the movements are gradually lost and the hip joint is fixed in one position.
- Loss of Activities of daily living : As a result of the symptoms the patient finds it extremely difficult to perform day to day activities such as walking, sitting, squatting, climbing stairs or participation in recreational sports activities
Diagnosis
The disease process of avascular necrosis starts long before the symptoms appear, usually months to years. So early diagnosis of avascular necrosis becomes important to start early treatment. Unfortunately, most patients report when the disease is already in advanced stages with complete destruction of the joint. The attending doctor will usually perform the following
- History : A detailed account of the preceding events and symptoms such as pain, stiffness and restriction of motion. Patient’s day to day activities, requirements and the past medical history
- Physical examination and tests: Attending doctor will perform a detailed physical examination including tests to see the movements of the hip which are restricted. A detailed examination of the other hip and joints.
- Blood tests: A complete blood profile and special blood investigations
- Radiograph : An X-ray of both the hips is done. Other than ruling out fractures an x ray usually details about the joint collapse, osteoarthritic changes, areas of bone destruction and new bone formation. Radiographs are best to detect changes when the disease has already advanced.
- MRI : It offers early detection even before the symptoms appear. Entailing the details of the tissues forming and surrounding the joint. Cartilage destruction, bone marrow and segments involved are easily detected.
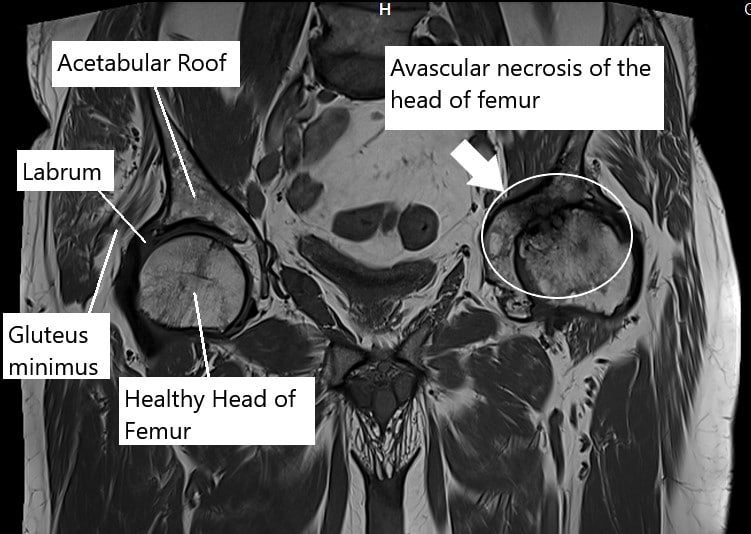
MRI showing AVN hip
Any infections or edema(swelling) in the joint is also visualized. Any changes in the other hip which might get involved in the future can be detected.
- Bone scan : A small amount of radioactive dye is injected which gets accumulated in the areas of excessive destruction or repair. The dye is visualised using special imaging scanners. It offers the earliest detection of disease process of osteonecrosis
Treatment
Early stages of disease are relatively pain free. The patient usually presents to the physician in the late stages with advanced collapse. Although if detected in early stages medical treatment can be helpful.
Non surgical treatment
Drug therapy includes use
- Lipid lowering drugs : These drugs are useful in people with high blood lipids/cholesterol
- Nonsteroidal anti-inflammatory medications : They provide symptomatic relief of pain and helpful to control the swelling in the joint. Although symptomatic they provide good relief in pursuing day to day activities. The disease process is not stopped.
- Anti-osteoporotic drugs : Drugs such as alendronate help to decrease bone loss and pain associated with it.
- Blood thinners : Drugs like warfarin are also used to prevent clots blocking the blood vessels.
- Physical therapy and precautions : Avoiding weight bearing on the affected limb slows down the collapse and physical therapy helps to maintain active range of motion.
Regardless, despite the medical treatment, the disease progresses in the majority of patients requiring surgical interventions.
Surgical management
Surgical interventions depend on the patients age, the segment of bone affected and the stage of the disease. Some of the various interventions are:
- Core decompression
Multiple drills are done in the hip bone to reduce the pressure inside and potentially allowing the bone forming cells to lay down new bone replacing dead bone. The reduced pressure allows for increased blood supply to the bone. The procedure is helpful when performed before the collapse of bone and cartilage.
- Vascularised and non-vascularized grafts
An attempt is made to reestablish the blood supply of the hip bone by inserting a bone graft taken from another part of the body. Usually a part of fibula bone(one of the two leg bones) along with its blood vessel is used as a graft. The grafted bone incorporates into the hip bone and with its blood supply helps in revascularization.
The grafts can also be non vascularized(without a blood vessel). Grafted bone not only provides structural support but also supplies potential bone forming cells which creep in substituting the dead bone. Muscle pedicle grafts can also be used. Again the procedure is helpful only if performed in early stages of the disease process.
- Osteotomies
These are surgeries which change the segments of the ball of the hip which bear weight. The diseased segment is surgically rotated so that the healthy segment comes to lie under the weight bearing portion and relieves the pain and stiffness. The diseased unloaded segment potentially starts to get healthy. The surgery is useful in smaller lesions.
- Total hip replacement/Hip resurfacing
Majority of patient report to the physicians when in pain and the disease process is already in advanced stages.
Total hip replacement is the best surgical option which not only relieves pain and stiffness but offers a faster rehabilitation usually 8 weeks. The patient rapidly goes back into his daily activities as before the disease. It involves replacing the hip joint with a prosthetic/artificial joint which recreates the movements and biomechanics of the normal joint. It offers a normal lifestyle even in advanced stages.
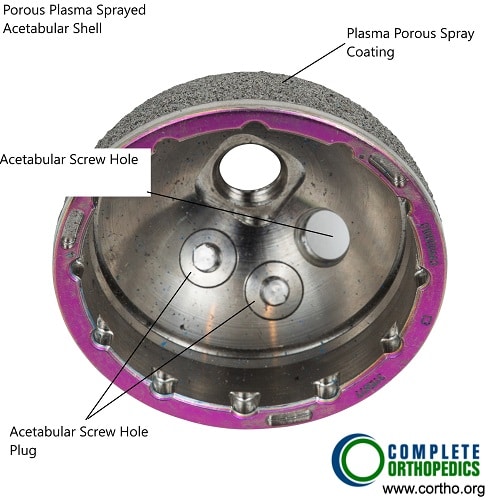
Metallic Acetabular shell
The acetabular shell is usually made of cobalt chromium alloy and consists of an outer porous coating. The porous allows the bone ingrowth into the surface as the prepared surface of the acetabulum heals. The acetabular shell contains holes for screw fixation. The screw holes are covered using screw plugs. The circumferential grooves help to firmly fix the acetabular liner in the shell.
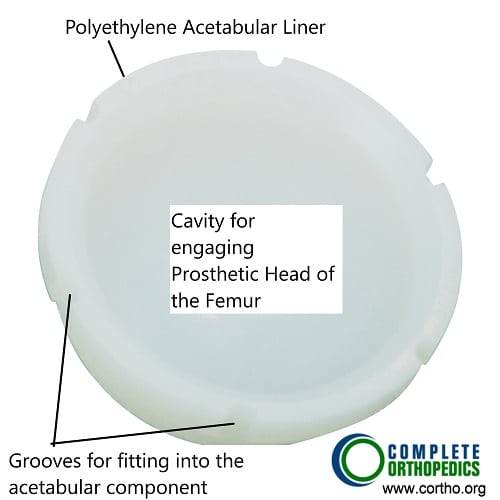
Acetabular liner
The acetabular liner is made of a specialized plastic known as highly cross linked polyethylene. The polyethylene is processed so provide a smooth surface for the head of the femur to moves in the cavity while decreasing the wear and tear of the implant.
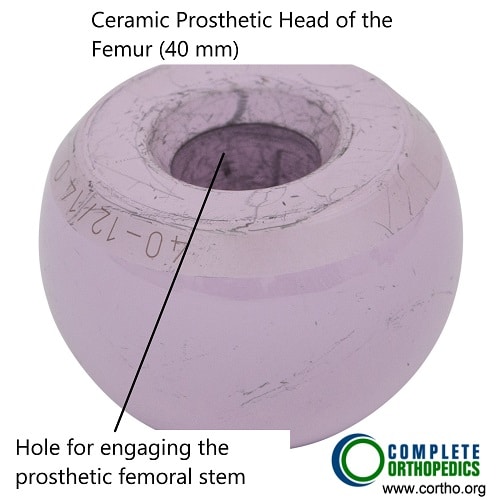
Ceramic prosthetic head of femur
The head of femur is replaced by a prosthetic head that may be made of cobalt chromium alloy or ceramic. The head is designed in a way to provide maximum smoothness on the surface to decrease friction. The surgeon plans to use the maximum diameter of the head according to the patient anatomy to prevent dislocation.
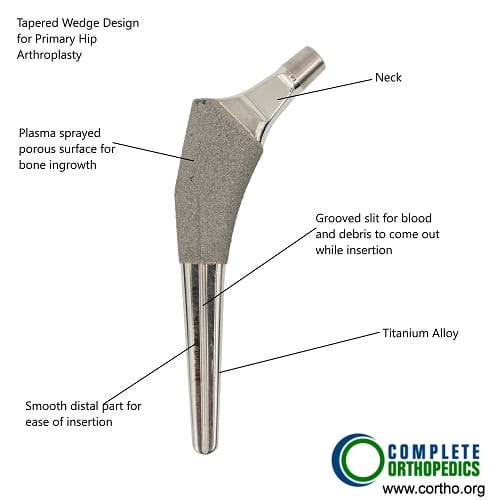
Wedge tapered prosthetic femoral stem
The prosthetic femoral stem is inserted in the upper part of the femoral canal. The stem is usually press-fitted in the femoral canal. The upper part of the prosthesis consists of a porous coating that helps bone ingrowth for firm fixation. The lower end is tapered for smooth insertion of the stem. The stem used for primary hip replacement is shaped for maximum bone preservation and to transfer the load distally.
November 29th is celebrated as Avascular Necrosis (AVN) Awareness day!
Do you have more questions?
What steps can individuals take to advocate for themselves and ensure they receive comprehensive care for avascular necrosis, including access to specialist care and ongoing monitoring?
Individuals with avascular necrosis can advocate for themselves by seeking care from healthcare professionals experienced in managing the condition, educating themselves about treatment options, and actively participating in their treatment plan. It’s essential to communicate openly with healthcare providers, ask questions, and seek second opinions if necessary to ensure comprehensive care.
Are there any emerging treatments or research advancements in the field of avascular necrosis that show promise for improving outcomes or reducing disease progression?
Researchers are continually exploring new treatment modalities and research advancements in avascular necrosis, including stem cell therapy, gene therapy, and tissue engineering techniques. While these approaches are still in the experimental stages, they hold promise for future treatment options.
What are the psychological impacts of living with avascular necrosis, and are there support resources available for affected individuals and their families?
Living with avascular necrosis can have significant psychological impacts, including anxiety, depression, and feelings of isolation. Support resources such as support groups, counseling services, and online forums can provide valuable emotional support for affected individuals and their families.
Can avascular necrosis affect children or adolescents, and if so, how does the condition manifest differently in younger individuals?
Avascular necrosis can occur in children or adolescents, typically as a result of trauma, infection, or underlying medical conditions. The condition may manifest differently in younger individuals and may require specialized treatment approaches.
What are the long-term implications of avascular necrosis, particularly in terms of joint degeneration and the need for additional surgeries?
Avascular necrosis can lead to progressive joint degeneration, which may necessitate additional surgeries such as revision hip replacement. Long-term follow-up care is essential to monitor joint health and address any complications that may arise.
Are there any restrictions or limitations on physical activity or exercise for individuals with avascular necrosis, particularly following surgical intervention?
While individuals with avascular necrosis may need to modify their physical activity level, especially during flare-ups or recovery periods, many can still engage in low-impact exercises such as swimming, walking, or cycling. However, high-impact activities may need to be avoided to prevent joint stress.
How does avascular necrosis impact the overall quality of life for affected individuals, particularly in terms of physical function and emotional well-being?
Avascular necrosis can significantly impact an individual’s quality of life by causing pain, mobility limitations, and emotional distress. However, with appropriate treatment and support, many individuals can maintain a good quality of life and continue to engage in meaningful activities.
Is there a genetic component to avascular necrosis, and are certain individuals more predisposed to developing the condition?
While avascular necrosis is not typically considered a hereditary condition, certain genetic factors may increase an individual’s susceptibility to developing the condition. Further research is needed to understand the genetic contributions to avascular necrosis fully.
Can avascular necrosis spontaneously resolve without medical intervention, especially in its early stages?
In some cases, avascular necrosis may stabilize or improve without medical intervention, particularly in its early stages. However, spontaneous resolution is rare, and most cases require medical management to prevent further progression.
Are there any alternative or complementary therapies that may help manage symptoms or improve outcomes for individuals with avascular necrosis?
Some individuals may find relief from complementary therapies such as acupuncture, chiropractic care, or herbal supplements. However, it’s important to consult with a healthcare professional before trying any alternative therapies.
How can individuals with avascular necrosis manage pain and discomfort on a day-to-day basis?
Pain management strategies may include medication, physical therapy, heat or cold therapy, and assistive devices to reduce joint stress. It’s essential for individuals to work closely with healthcare professionals to develop a personalized pain management plan.
Are there any dietary or nutritional recommendations for individuals with avascular necrosis to support bone health?
While there are no specific dietary recommendations for avascular necrosis, maintaining a balanced diet rich in calcium, vitamin D, and other essential nutrients may support overall bone health.
What is the prognosis for individuals with avascular necrosis, particularly if the condition is diagnosed in advanced stages?
The prognosis varies depending on factors such as the extent of bone damage, the effectiveness of treatment, and the patient’s overall health. Early diagnosis and appropriate treatment can help improve outcomes and quality of life.
Are there any preventive measures or screening tests available for individuals at risk of avascular necrosis?
Currently, there are no specific preventive measures or screening tests for avascular necrosis. However, early detection and management of underlying risk factors may help reduce the risk of developing the condition.
What lifestyle modifications can individuals make to reduce their risk of developing avascular necrosis?
Lifestyle modifications may include avoiding excessive alcohol consumption, maintaining a healthy weight, avoiding prolonged use of steroids, and managing underlying medical conditions that affect blood flow.
Can avascular necrosis affect other joints in the body besides the hip joint?
Yes, although avascular necrosis commonly affects the hip joint, it can also occur in other weight-bearing joints such as the knee, shoulder, and ankle.
Is there a difference in recovery time and rehabilitation between non-surgical and surgical treatment options for avascular necrosis?
Yes, surgical interventions often require a longer recovery period and more intensive rehabilitation compared to non-surgical treatments. However, the long-term benefits of surgery may outweigh these considerations.
What are the risks and potential complications associated with surgical interventions for avascular necrosis?
Risks may include infection, blood clots, implant failure, nerve injury, and postoperative stiffness. However, these risks are mitigated with careful preoperative evaluation and surgical technique.
How effective is total hip replacement in relieving pain and restoring function in patients with advanced avascular necrosis?
Total hip replacement is highly effective in relieving pain, restoring mobility, and improving quality of life in patients with advanced avascular necrosis. It involves replacing the damaged hip joint with an artificial prosthetic joint.
What surgical interventions are commonly performed for advanced cases of avascular necrosis?
Surgical options may include core decompression, bone grafting, osteotomies, or total hip replacement. The choice of surgery depends on factors such as the extent of bone damage and the patient’s overall health.
What treatment options are available for avascular necrosis, particularly in the early stages of the condition?
Non-surgical treatments may include medication (e.g., lipid-lowering drugs, anti-inflammatory drugs), physical therapy, and lifestyle modifications. Early intervention with medications and activity modifications can help slow disease progression.
How is avascular necrosis diagnosed, and at what stage is it typically detected?
Diagnosis involves a combination of medical history, physical examination, blood tests, X-rays, MRI scans, and bone scans. Unfortunately, it is often detected in advanced stages when symptoms become apparent.
What are the common symptoms experienced by individuals with avascular necrosis of the hip joint?
Common symptoms include hip pain, stiffness, limping, restricted range of motion, and difficulty performing daily activities.
Are there specific risk factors or predisposing conditions that increase the likelihood of developing avascular necrosis?
Yes, several factors such as trauma, alcoholism, steroid abuse, blood disorders, chronic liver disease, certain medications, and congenital diseases can increase the risk of avascular necrosis.
How does avascular necrosis of the hip joint impact bone health and function?
Avascular necrosis disrupts blood supply to the hip joint, leading to bone death (necrosis) and subsequent joint deterioration. This can result in pain, stiffness, and loss of mobility.


