Case Study: Open Repair of Tendon-Achilles Tendon
using Fiber Tape and SwiveLock in a 32 year-old male
This suture contains a long-chain polyethylene structure, similar to Fiberwire® suture. Its large footprint makes it appropriate for repairing degenerative cuff tissue where tissue pull-through is a concern.
SwiveLock anchors are intended for use in repair and reconstruction techniques with Suture Tape, Fiber Wire®, Fiber Tape®, and soft-tissue grafts.
A 32-year-old male patient visits the office with complaints of pain behind his ankle and inability to put weight on it on the left side. He states it started two weeks ago when he was playing football. He is working for USPS.
Associated Symptoms: no numbness; no tingling; no swelling; no redness; no warmth; no ecchymosis; no catching/locking; no popping/clicking; no buckling; no grinding; no instability; no radiation down leg; no drainage; no fever; no chills; no weight loss; no change in bowel/bladder habits; no tenderness to touch however, it has weakness and pain with motion.
Because of the pain he experienced, we agreed to do an MRI to know where the pain was coming from.
MRI were reviewed and discussed, the soft tissues have significant posterior soft tissue swelling and edema secondary to Achilles tendon pathology. The bone marrow has a mild edema in the anterior tibial plafond and. No fracture or avascular necrosis.
While the osteochondral lesion is none, the medial tendons-posterior tibialis tendinosis and tenosynovitis without tears and the remainder the medial tendons, anterior tendons and lateral tendons are unremarkable.
The lateral ligaments: Syndesmotic ligaments: evidence of remote sprain and thickening of the anterior tibiofibular Ligament. No acute syndesmotic injury. Anterior talofibular ligament: evidence of remote sprain with mild thickening and scarring but no acute injury.
Calcaneofibular ligament and Posterior talofibular ligament are unremarkable. Medial ligaments: Deltoid ligament, Tibio-spring ligament, Proper spring ligament are unremarkable. Lisfranc ligament and joint are both normal.
The Achilles Tendon: Full-thickness tear of the Achilles tendon 4.3 cm proximal to its attachment near the myotendinous junction/aponeurosis with significant underlying, the Tendinosis and marked thickening of the Achilles tendon with a 1 cm gap in the torn tendon fibers.
The Plantar Aponeurosis: Thickening of the central cord of the plantar aponeurosis without Edema compatible with the sequelae of prior plantar fasciitis which is now healed. Sinus Tarsi: Normal fat signal characteristics. Tarsal Tunnel: Normal without masses. Muscles: Normal signal and bulk without edema or atrophy.
Marked Achilles tendinosis with a full-thickness tear 4.3 cm proximal to its attachment at the myotendinous junction with a 1 cm gap and associated soft tissue swelling. Posterior tibialis tendinosis and tenosynovitis without tears.
Evidence of remote syndesmotic ligament sprain and remote anterior talofibular ligament sprain but no acute ligamentous injury. Sequelae of healed plantar fasciitis.
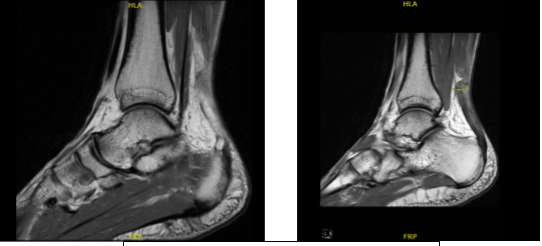
MRI-1.2T Left ankle non-contrast
Upon the examination, we discussed treatment options including operative and nonoperative management. The patient opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, nonhealing, need for repeat surgery, ankle stiffness, need for rehabilitation, systemic complications including blood clots, cardiac, pulmonary, neurological complications including death.
The patient understood and signed an informed consent.
The patient was taken to the operating room where general anesthesia was induced on the bed. The patient was turned prone and put in a well-padded position. Bolsters were used for padding of the chest. Silicone pads were used under the kneecaps. All the bony prominences were well padded.
The right lower extremity was put in traction on a bolster. The left lower extremity was prepped and draped aseptically in the usual fashion. Preop antibiotic was given. Tourniquet was elevated. A time-out was called.
A posterior incision just medial to the midline was given. Skin and subcutaneous tissue were cut in the line of incision with sharp dissection. Paratenon was reached and it was split along the line of the incision.
The tear could be felt and delivered out of the wound with manual separation. The wound edges were cleaned. The wound was irrigated. A 1.3 mm Fiber Tape was used to pass Krakow sutures with bites from either side x2 making a four-tailed repair of the proximal tendon.
Stab incisions were given over the calcaneus and Banana Suture Lasso was passed on either side of the tendon-Achilles insertion. The lasso was brought through the substance of the tendon-Achilles and through the distal stump and delivered at the operative site.
Suture Lasso was used to deliver the Fiber Tape one from each side on to either side. Once the Fiber Tapes were delivered, the reduction was checked and found to be satisfactory.
The Fiber Tapes were put into the calcaneus on either side after drilling and tapping a hole for 2.75 mm Swive Lock at a 45:45-degree angle into the calcaneus. The final fixation was checked after tagging with SwiveLock and found to be very satisfactory.
A circumferential closure over the repair was done using #0 Fiber Wire. Wound was again washed and irrigated. Paratenon was closed using Vicryl. Closure was done using #2-0 Vicryl and # 4-0 Monocryl. Tourniquet was released.
Dressing was done using Adaptic, 4 x 8, Webril, splint, and Ace wrap. The patient was turned supine and extubated and moved to the Recovery in stable condition.
After two weeks of the patient being seen for his post-operative visits, we discussed the treatment options, we have decided to continue with ice and elevation of the ankle to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. He will be NWB with axillary crutches. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
Aspirin continues for a total of 28 days since surgery for DVT prophylaxis. We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in 10 days’ time to evaluate their progress and application of wedged cam walker boots.
The 10 days were done, the patient was here for his 3-week post op appointment of left ankle. We discussed the treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now.
Physical Therapy to be started, we advised the patient to use Ice and elevation to lessen the swelling, an OTC as an anti-inflammatory meds and follow up checkup after 4 weeks. After a month the patient visits for his follow up checkup, the patient is doing well after the surgery, and has weaned off wedges.
He is also able to walk without boots. He wants to go back to work on light duty and he denies pain, fever, chills. With the continued follow up checkup the patient showed progress from time to time he visits the office. He gets well after the surgery and with the help of continuing physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
