Case Study: Arthroscopy: RCR and Subacromial
Decompression of the Shoulder in a 53 year-old male
Surgery called acromioplasty is used to address rotator cuff disease and impingement of the shoulder. Acromioplasty, also known as shoulder subacromial decompression, is a surgical treatment used to treat shoulder impingement and as a follow-up to rotator cuff repair (RCR).
A 53-year-old, driver, male patient presents with bilateral shoulder pain due to a motor vehicle accident. He had a car accident in 2020 in which he injured the right shoulder.
The right shoulder showed a rotator cuff tear but he improved to normal without surgery. His right shoulder has started bothering again after this accident in 2021. He is not able to sleep due to pain.
His Xray showed no dislocation but has mild to moderate arthritic change with suggestion of rotator cuff degeneration. We agreed to have an MRI and it showed a complete tear of the rotator cuff associated with the distal anterior supraspinatus tendon. Aside from this also found a partial tear of the rotator cuff proximal supraspinatus tendon. Prominent joint and bursal effusions.
We talked about the patient’s diagnosis and the treatment choices available, which included managing the extremity as it is, structured workouts, medications, injections, and surgical possibilities. Along with the anticipated risks and benefits, we also talked about the nature and purpose of the available treatment options.
Surgery has been requested by the patient, and I believe that is a viable choice. I talked at length with the patient about the hazards that are inherent and unavoidable, including anesthesia, infection, damage to the nerves and blood arteries, blood loss, blood clots, and even death.
We also discussed the potential inability to resume previous activities or employment, the requirement for additional surgery, and complex regional pain syndrome. The patient is also aware that a protracted rehabilitation period usually follows a surgical operation.
We discussed the possibility that not all of the discomfort could be relieved. I also mentioned that there is no assurance that all the strength and function will return. Additionally, the patient is aware of the dangers of re-tear or failure to heal.
The patient is aware that implants might be used in this procedure. The patient has decided to go forward with the procedure despite acknowledging these dangers. There was plenty of time for questions, many of which were answered.
We have talked about the surgical process as well as reasonable expectations for the risks, results, and postoperative instructions. The patient understood and signed an informed consent.
The patient was taken to the operating room where supraclavicular block was given under sedation. General anesthesia was induced. The patient was put in a lateral position with the right shoulder up. Preoperative antibiotic was given. Preoperative tranexamic acid was also given. The right shoulder was prepped and draped aseptically in the usual fashion.
Entry portal was made through the posterior soft spot. Arthroscope was inserted into the glenohumeral joint. Anterior and superior entry portal was made with the use of the spinal needle.
Examination of the glenohumeral joint showed a large rotator cuff tear. It also showed partial tearing and inflammation of the biceps’ tendon. Decision was made to not do the biceps and do a mini-open biceps tenodesis later.
Examination of the cartilage showed grade 1 osteoarthritic changes of the glenoid surface. There was fraying of the labrum, which was debrided with the use of a shaver. There was fraying of the subscapularis tendon, which was also debrided with the use of the shaver.
The arthroscope was inserted into the subacromial space. Subacromial bursectomy was performed with the shaver. This was followed by acromioplasty with the use of Coblation wand followed by a 6.0 burr incising the acromial spur, osteoarthritis of the AC joint was also present, which was again cleaned with the use of a Coblation wand followed by 6.0 burr excising about a centimeter of the distal clavicular through the posterior as well as anterior superior portal.
A lateral entry portal was made for the repair of the rotator cuff. The debridement of the rotator cuff was done. Also, the superior surface of the head of humerus was cleaned and debrided with the use of burr for the preparation for the repair of the rotator cuff.
Triple play Corkscrew bioabsorbable corkscrew from Arthrex was used and inserted into the head of the humerus. The six tails of the three sutures of the anchor were passed through the rotator cuff tendon sequentially and tied on to each other in the form of the horizontal mattress.
Good apposition and repair of the rotator cuff was achieved. The sutures were cut. Final pictures were taken and saved. The shoulder was thoroughly irrigated and drained. Arthroscope was removed and the patient’s arm was taken out of traction. A subpectoral approach was planned for the biceps tenodesis.
A decision about 2.5-cm incision was given along the Inferior margin of the pectoralis tendon in the anterior axillary port. The deltopectoral fascia was cut in the line of the incision. The blunt dissection was performed under the pectoralis major tendon to reach the bicipital groove and biceps tendon.
A periosteal elevator followed by Hohmann’s was used to retract the pectoralis major laterally. The right-angle forceps was used to deliver the biceps tendon. The whip stitches were done into the biceps’ tendon with the use of FiberLoop. Excess of the tendon was cut.
Tendon was marked on to the bone for a proper tension on tenodesis and a bicortical Beath pin was inserted into the bicipital groove. This was followed by proximal unicortical reaming of the humerus in the bicipital groove. The whip stitches of the tendon were loaded and were passed bicortically and slipped.
The sutures were tightened and the tendon would be seen and bring the biceps into the humerus. The sutures were tied on to each other after passing through the tendon trice. Interference screw was tried to be inserted, but could not be done because of the loosening into the hole.
Fixation of the biceps’ tendon was achieved with the help of the buttress. The wound was thoroughly irrigated and drained. Closure was done with the use of #0 Vicryl, #2-0 Vicryl, and # 3-0 Monocryl.
The arthroscopic portals were closed with the use of # 3-0 nylon. Dressing was done with the use of Xeroform, 4×4’s, ABD, Medipore tape. The patient was put in the shoulder immobilizer, extubated, and moved into the bed in stable condition.
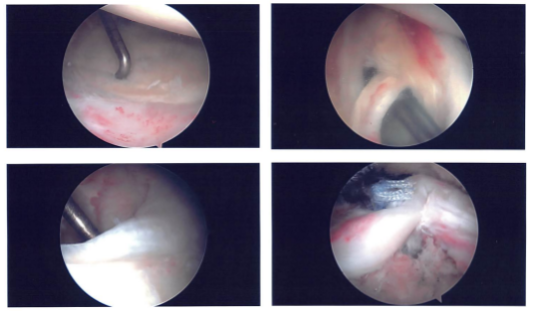
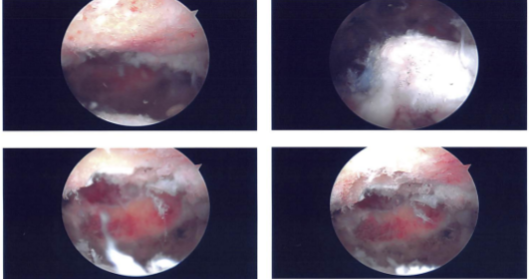
Intraoperative images
After one week the patient was seen in the office for his postoperative visit no x-rays were required and he denies fever and chills. The patient has an allergic reaction to Cephalexin and he may need Left RCR also in the future.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the shoulder. We went over the arthroscopic pictures and removed the stitches during the visit.
We will continue with ice and elevation of the shoulder to decrease swelling and pain. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate his progress.
After two weeks the patient is here for his postoperative visit, no x-rays were needed. He denies fever and chills and he had an allergic rash to keflex which has resolved now and he is not using the abduction pillow. The patient’s follow up checkup in 2 weeks.
After a month the patient visits the office for his follow up checkup, no x-rays were needed, he does not have fever or chills. He is without the immobilizer and complains of pain in the shoulder early in the morning.
She takes NSAIDs for pain. He has stiffness in the right shoulder, he is working with PT and he is improving gradually. With continued physical therapy, the patient gets well after the surgery.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
