Case Study: Partial Medial Meniscectomy
and Microfracture Surgery of Patella left knee
performed to a 58-year old female patient
An essential diagnostic and treatment aid for the management of knee disorders is knee arthroscopy. Meniscectomy, loose body removal, chondroplasty, microfracture, irrigation and debridement, and tendon reconstruction are examples of indications. In this set of articles, we provide an in-depth analysis of partial medial meniscectomy and microfracture surgery of Patella.
Patient is a 58-year-old male with complaint of left knee pain for over a year now. The pain is moderate in intensity. Patient describes the pain as stabbing and throbbing. The pain is constant and does in sleep. The pain is associated with twisting or bending. Patient is currently working as a stagehand which involves a lot of physical activity.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line, and has an effusion. Patient also has PF crepitus and tenderness on palpation along the medial and lateral PF joint line. Patellar grinding test is positive.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion, but have full extension. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present.
X Ray reports were presented and there are no significant degenerative changes. The patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 7cc of 1% lidocaine and 80 ml of depo-Medrol were injected into the left knee jt.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
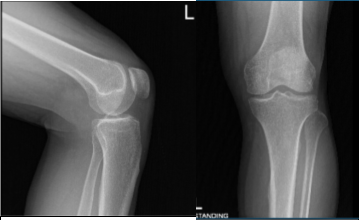
AP and Latera View
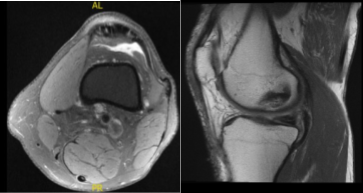
The patient got a cortisone injection, which helped him transiently but the pain came back. There is mild mucoid degeneration of the anterior cruciate ligament. There is mild proximal medial collateral ligament sprain with associated periligamentous soft tissue edema which extends along the posteromedial capsule.
There is mild popliteus insertional tendinosis. We discussed the treatment options and the patient opted for surgical management, including risks and complications of surgery and need for cortisone injection and PT as well.
General anesthesia induced the patient; a tourniquet was put on the lower thigh on the left side. The left knee was put into a knee holder. Aseptic prep and draping were performed. Preoperative antibiotic was given.
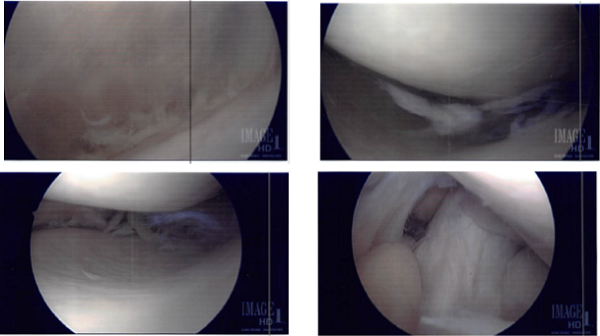
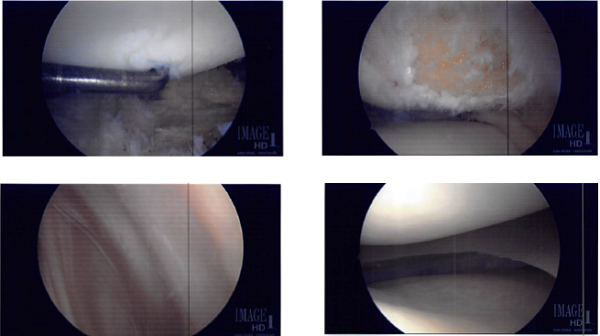
The tourniquet was inflated. Lateral entry portal was made and the scope was entered. Osteochondral OA grade 3 to grade 4 damage was found on the lateral inferior patella. Lot of debris was found in the knee as in the suprapatellar pouch and medial gutter.
The knee scope was moved to the medial compartment where a lot of debris as well as medial meniscus tear could be seen. medial entry portal was made. A probe was entered and meniscal tear were examined and pictures! was taken.
A shaver was inserted to clean off the debris as well as margins on the medial meniscus. The final balancing of the medial meniscus was performed. The lesion was also debrided. Microfracture of patellar osteochondral defect was done using pigtail punches and subchondral fat globules could be seen from the microfracture site.
The wound was lavage using copious amounts of normal saline. Scope was removed. Closure was performed using #4-0 nylon; 20 cc of 0.5% ropivacaine was injected into the knee.
Dressing was done using Adaptic, 4×4 and ABO along with web roll and Ace wrap. Tourniquet was released. The patient was extubated and moved to the postoperative area unit in a stable condition.
Intraoperative Images from start to final process
After two weeks, the patient was seen in the office and we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during today’s visit. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
The Patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.