Case Study: Medial and Lateral Meniscus Repair and
ACL Reconstruction performed to male athlete patient
The most common soccer injuries include sprains, muscle strains, anterior cruciate ligament (ACL), and meniscus tears. Women are considerably more vulnerable to harm because they have an Access Control List (ACL) damage rate that is four to eight times higher than that of men.
Soccer has one of the highest incidences of ACL rupture for both male and female players, especially in young athletes between the ages of 14 and 19. Female athletes have a higher risk of tearing their ACL (3 to 5 times that of a major knee injury) than male athletes.
Patient is 19 year-old-male patient with pain in his left knee. It started after he slipped while playing soccer at home. His X-ray were presented and reviewed, though there are no significant degenerative and no acute fracture.
His history and examination are strongly suggestive of ACL rupture with possible lateral meniscus tear left knee. Other symptoms were not present. Further diagnostic testing is required at this time. Patient will move his knee and be WBAT with crutches.
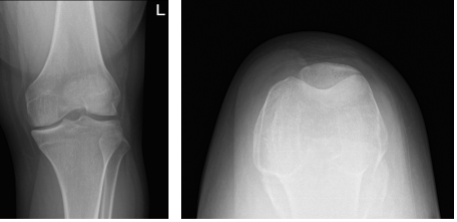
Left knee X-ray complete with patella
MRIs were reviewed and discussed with the patient and found significant results on his knee pain. Recent pivot shift injury resulting in a complete tear of the ACL and nondisplaced subchondral fractures at the lateral femoral condyle and lateral tibial plateau.
There are complex tears of both the medial and lateral menisci. A large displaced meniscal flap from the lateral meniscus extends into the meniscal tibial recess at the posterior horn/body junction. There is also mild cartilage loss in the lateral compartment and large joint effusion.
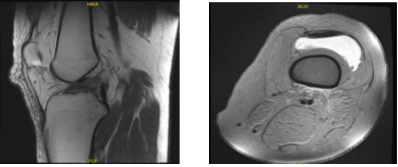
MRI-3T Left knee non-contrast
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and I think that is a reasonable option. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal.
The patient understands implants may be utilized during this surgery. The patient expressed understanding of these risks and has elected to proceed with surgery.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. Adductor canal block was given. A mid-thigh tourniquet was applied. Left lower extremity was prepped and draped in the usual fashion. A timeout was called.
Preop antibiotic was given. Esmarch was used to exsanguinate the limb and tourniquet was elevated to 300 mmHg. Lateral entry portal was made and an arthroscope was introduced into the knee joint. There was no osteochondral lesion of the patellofemoral joint, medial condyle, lateral condyle.
Examination of the medial meniscus showed a big body oblique vertical tear of the medial meniscus along with tear of the posterior horn of the medial meniscus. There was ACL tear, which was not repairable due to edgy mid-substance.
There was a lateral meniscus tear along the mid substance and anterior body of the lateral meniscus, which was flipped inside. Medial entry portal was made. Probe was introduced and the lateral meniscus tear was reduced with difficulty.
The lateral meniscus tear was held in place using a spinal needle, through which a Fiber Wire was passed. The FiberWire was used as a holding suture. Meniscal stitch from Arthrex were used x2 to repair the lateral meniscus.
Similarly, the medial meniscus was also reduced and sutured using two meniscal stitches from Arthrex. Fast-Fix chrome from Smith & Nephew was used for repair of the meniscal of the posterior horn. The repairs were satisfactory. Pictures were taken and saved.
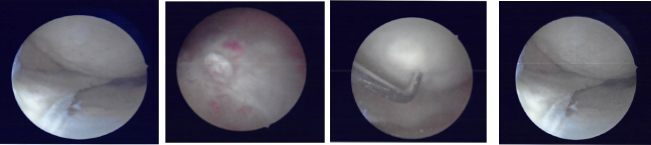
Intraoperative Arthroscopic Images
Now, the acquired tendon graft was harvested through a 3-cm incision. The tendon was prepped on the back table and FiberWire with the FiberTak was used to length of the graft was 80 mm. The graft was marked at 35 mm on the femoral side. The Intercondylar notch was prepped for ACL Insertion.
The entry portal was made using the guide. Lateral exit point was marked through the guide and incision given. The was inserted and a Flip Cutter was inserted from the lateral condyle towards the femur. When it came into the medial condyle, the guide was removed and the cutter was flipped.
About 30 mm tunneled was made on the femoral side with the FlipCutter. Similarly, the tibial footprint was cleaned and a tibial tunnel was made with an ACL guide. The Flip Cutter was used to make a total of 75 mm. Crosswood cannula was inserted on the medial portal for easy suture management and Anvil.
Once the tunnels were done, FiberLoop was passed on either side. The femoral side was brought out of the Crosswood along with Tightrope and passed through the femoral channel under arthroscopic visualization. Once 29 mm was crossed, the tibial loop was extracted and the tibial Tightrope was passed.
Once the tibial TightRope was out of the bone, the button was flipped and tightened. Similarly, the button was flipped on the femoral side and tightened. Sequential tightening was done on the tibial and femoral site for the TightRope.
After a week of seeing patients, he has been improving with regards to pain and swelling. He is limping and has been using crutches for ambulation. Denies fever, chills, reinjury. After two weeks post surgery the incisions are healing well, without evidence of drainage, erythema or warmth.
There is a full range of motion without discomfort. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
