Minimal Invasive Spine Surgery
Many patients are a good candidate for Minimal Invasive Spine Surgery (MISS). They can be benefitted by the recent advancements in spine surgery as well as minimal invasive techniques. MISS can be of various types viz. Tubular, endoscopic, microscopic, percutaneous but the important information is as to which can take care of the disease completely.
Advantages of MISS include smaller incisions and scars, decreased pain, reduced blood loss, shorter hospital stay, lower infection rate and early recovery. Through MISS, a varied procedure including laminectomy, discectomy as well as fusion can be performed. MISS has its own disadvantages also including need of skilled surgeon, increased radiation exposure during surgery, dependency on technology and increased cost.
Example of MISS in cervical spine are cervical microdiscectomy and ACDF. MISS in Lumbar spine can be used to perform discectomy, laminectomy as well as fusion.
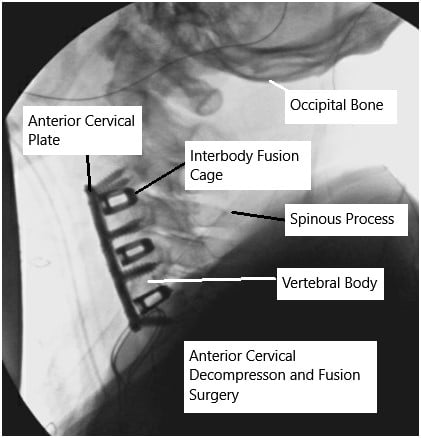
Intra-operative fluoroscopy image showing anterior cervical decompression and fusion.
MISS is performed through small incisions or a set of incisions. It is usually performed with the help of tubes or specialized retractors to have access to the spine while inflicting less damage to the surrounding skin, muscles and soft tissue.
The patient may need multiple small incisions in the midline or on either side so as to allow access to the spine. The surgery requires specialized instrumentations, retractors as well as illumination with light aids. It may also involve the use of operating microscopes to enhance the visualization as well as optics. The implants that are used in minimal invasive spine surgery like the screws and rods are different from the one used in routine surgeries as they need manipulation and placement through small incisions and a minimal invasive approach.
Recent advances of use of navigation during surgery has also helped in certain complex surgeries. In these a real time imaging at the time of surgery helps in better understanding the anatomy and allow accurate placement of instrumentation.
PREOPERATIVE WORKUP
The patients are usually seen by the physician and appropriate preoperative investigations including advanced imaging, blood work and ECG and chest x-rays as needed are done. The patients may also need clearance from their primary care physician and anesthesiologist before the surgery. The patients are instructed to come to the hospital two hours in advance. The patients are taken to the preoperative area where they are seen by the anesthesiologist and appropriate procedure performed before the patient is taken to the operating room. In the operating room the patient usually is given general anesthesia and intubated before being positioned for the surgery.
POSTOPERATIVE CARE AND RECOVERY
The patients who undergo lumbar spine surgery are usually extubated after the surgery. Depending on the procedure and recovery form surgery, patient can be discharged home on the same day if they meet the criteria to discharge. Patients can mobilize in and out of bed with or without a back support depending on the surgery and recovery from anesthesia. Immediately after the surgery, the patients are encouraged to do their activities of daily living from the first postop day. The patients are provided with medications in the hospital as well as for home to take care of pain and muscle spasms that can develop after the surgery. Incisions need to be kept clean and dry. The patients are instructed to avoid bath and hot tubs, swimming, heavy lifting, driving and smoking. The patients can take shower and remove the dressings after 72 hours from surgery and replace it with dry dressing. The patients are advised to eat healthy and nutritious diet with lot of fibers. The patients are also instructed to use over-the-counter laxatives for constipation that may develop due to pain medications.
RISKS AND COMPLICATIONS
As for all surgeries there are certain but rare risks for anesthesia including cardiac arrest, stroke, paralysis, and rarely death.
- Risks of Spine surgery may include though not limited to:
- Hematoma or hemorrhage
- Damage to the major vessels which may result in excessive bleeding, even death
- Blindness
- Damage to the dura, resulting in a cerebrospinal fluid leak
- Damage to vital structures around the neck
- Failure, loosening or pull out of the cage, graft, rod or screws
- Wound infection
- Failure of fusion to happen
- Damage to the nerve root(s) resulting in new onset or deterioration of preexisting pain, weakness, paralysis, loss of sensation, loss of bowel or bladder function, impaired sexual function, etc., which may or may not recover.
- A few of these conditions may warrant repeat surgery
Certain patient population is at a higher risk for complication which include but are not limited to:
- Smoking
- Seizures
- Obstructive sleep apnea
- Obesity
- High blood pressure
- Diabetes
- Other medical conditions involving your heart, lungs or kidneys
- Medications, such as aspirin, that can increase bleeding
- History of heavy alcohol use
- Drug allergies
- History of adverse reactions to anesthesia
WHEN TO VISIT AN EMERGENCY ROOM AFTER A SURGERY:
- Suspected cardiac problem: severe chest pain or pressure, shortness of breath, tightness in chest, pain in left arm, jaw pain, dizziness or fainting, unexplained weakness or fatigue, rapid or irregular pulse, sweating, cool, clammy skin, and/or paleness\
- Suspected Stroke: trouble speaking, changes in vision, confusion or other change in mental status
- \Suspected venous thrombosis: swelling of the legs, ankles, or feet, discomfort, heaviness, pain, aching, throbbing, itching, or warmth in the legs, sudden shortness of breath, chest pain, coughing up blood, rapid or irregular heart rate
- Suspected Sepsis: high grade fever, with shivers associated with fatigue, dizziness, racing heart, pale or discolored skin, sleepy, difficult to rouse, confused, short of breath
• Heavy bleeding from the surgical site - Severe allergic reaction with trouble breathing, swelling, hives
WHEN TO CONTACT A DOCTOR’S OFFICE AFTER SURGERY:
- temperature more than 101 degrees Fahrenheit
- increased pain or tenderness near the incision
- poor pain relief
- signs of infection: increased swelling, redness, increased drainage, increased warmth, pus, foul smell, bleeding at the incision, incision coming apart
• increased numbness, numbness in genital area - inability to feel or move fingers or toes
- pale blue, white or abnormally cold fingers or toes
- nausea (upset stomach) or vomiting (throwing up) that won’t stop
- increased tiredness
- a generally worse feeling than you had when you left the hospital
- problems urinating, severe constipation or severe diarrhea
- a concern about any other symptoms that seem unusual
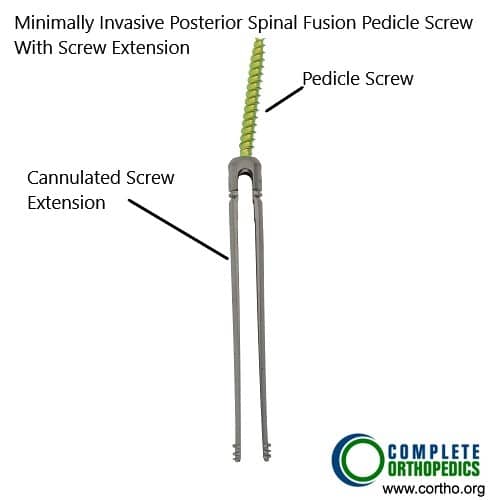
Pedicle screw with cannulated screw extension for minimally invasive posterior spine fusion
The image shows pedicle screws used in the minimally invasive posterior spinal fusion. The screw extensions aid in the insertion of the screw through key-hole incision.

Rods used in minimally invasive posterior spinal fusion
The rods are attached to the pedicle screws for achieving stability across the involved spinal segments. The rods in the image above are designed for minimally invasive posterior spinal fusion.
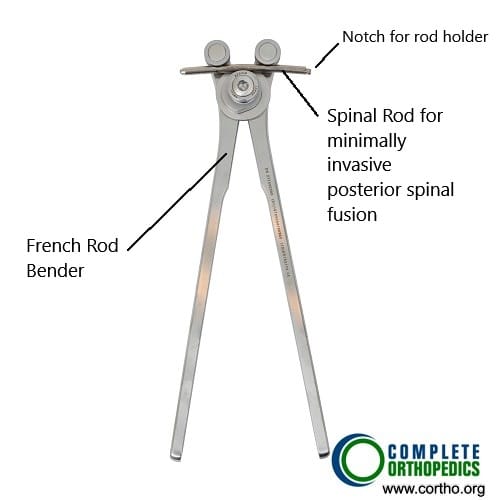
French rod bender
The rod bender in the image above is used to bend and contour the rod for insertion in the slot of the pedicle screws and to achieve maximum stability intra-operatively.
Do you have more questions?
What is minimally invasive spine surgery (MISS)?
Minimally Invasive Spine Surgery (MISS) is a surgical technique aimed at reducing tissue damage and recovery time compared to traditional open spine surgery. It uses smaller incisions and advanced technologies like endoscopes, navigation systems, and robotics.
What are the benefits of MISS over traditional open spine surgery?
MISS offers several benefits, including smaller incisions, reduced tissue damage, less blood loss, shorter hospital stays, quicker recovery times, and reduced postoperative pain and complications.
What conditions can be treated with MISS?
MISS can treat various conditions, including herniated discs, spinal stenosis, spondylolisthesis, spinal metastasis, spinal deformities, and spinal trauma.
How does endoscopic-assisted spinal surgery work?
Endoscopic-assisted spinal surgery involves using an endoscope to visualize the surgical area through small incisions. This approach minimizes tissue damage and preserves normal anatomy, leading to faster recovery.
What is the difference between MI-TLIF and traditional TLIF?
Minimally Invasive Transforaminal Lumbar Interbody Fusion (MI-TLIF) uses smaller incisions and a tubular retractor, whereas traditional TLIF involves larger incisions and more tissue disruption. MI-TLIF typically results in less blood loss and faster recovery.
What role do robotics play in MISS?
Robotics systems enhance the precision and reliability of spinal surgeries. They help surgeons perform delicate procedures more accurately and reduce physical and mental fatigue during long operations.
How do navigation systems improve the accuracy of MISS?
Navigation systems provide real-time, three-dimensional imaging during surgery, allowing surgeons to accurately place implants and perform procedures with greater precision and safety.
Are there any risks associated with MISS?
Like any surgery, MISS has risks, including infection, nerve damage, and complications related to anesthesia. However, these risks are generally lower compared to traditional open surgery.
How long is the recovery period after MISS?
Recovery time varies depending on the specific procedure and patient factors. Generally, patients undergoing MISS experience quicker recovery times and can return to normal activities sooner than those who have traditional open surgery.
Is MISS suitable for everyone?
Not all patients are candidates for MISS. Factors such as the type and severity of the spinal condition, patient health, and previous surgeries play a role in determiNot all patients are candidates for MISS. Factors such as the type and severity of the spinal condition, patient health, and previous surgeries play a role in determining eligibility.ing eligibility.
What advancements have been made in MISS technology?
Recent advancements include high-resolution endoscopic cameras, improved navigation and imaging systems, and robotic-assisted surgical tools. These technologies enhance the precision, safety, and outcomes of MISS.
How does MISS help in treating spinal deformities?
MISS is beneficial for spinal deformities as it reduces tissue damage, blood loss, and recovery time. Techniques like MI-TLIF and MI-LLIF provide sufficient correction while minimizing complications.
Can MISS be used for spinal metastasis?
Yes, MISS can be effectively used for spinal metastasis. It offers equivalent functional outcomes to traditional surgery with reduced morbidity, such as less blood loss and fewer infections.
What are the limitations of MISS?
Limitations of MISS include a steep learning curve for surgeons, potential for inadequate decompression in some cases, and higher costs due to advanced equipment.
How does MISS compare to traditional surgery in terms of outcomes?
Clinical outcomes of MISS are comparable to traditional open surgery, with additional benefits of reduced tissue damage, quicker recovery, and fewer complications.
What types of spinal implants are used in MISS?
MISS utilizes advanced spinal implants made from biocompatible materials that enhance stability and fusion. These include cages, rods, screws, and plates specifically designed for minimally invasive procedures.
What is the role of augmented reality (AR) in MISS?
Augmented reality (AR) provides surgeons with enhanced visualization of the surgical area, superimposing critical information over the patient’s anatomy in real-time, thereby improving accuracy and safety.
Can MISS be performed on patients with previous spinal surgeries?
MISS can be performed on patients with previous spinal surgeries, although careful evaluation and planning are required to address potential scar tissue and anatomical changes.
What is the role of fluoroscopy in MISS?
Fluoroscopy provides real-time imaging during surgery to guide the placement of instruments and implants, enhancing precision and safety.
What are the advantages of using navigation technology during MISS?
Navigation technology provides real-time imaging and guidance, allowing for more precise and safer placement of instrumentation.
What kind of implants are used in MISS?
Specialized screws, rods, and other implants designed for insertion through small incisions are used in MISS.
What should I do if I experience severe pain or complications after MISS?
Contact your doctor immediately if you experience severe pain, signs of infection, or any other concerning symptoms.
How does the surgeon decide which type of MISS technique to use?
The choice of technique depends on the specific spinal condition, the location and severity of the issue, and the surgeon’s expertise and assessment of the best approach for the patient.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
