Case Study: Medial Meniscectomy on the left knee
and Chondroplasty of the medial femoral condyle
in a 76 year-old male
Meniscectomy is a frequent orthopedic operation used to treat meniscal disease in the elderly population that causes knee discomfort. The most frequent knee injury is a torn meniscus. Individuals who have meniscus tears commonly experience mechanical knee problems.
People can report a popping, clicking, or locking sound when walking. Moreover, patients frequently experience painless or painful intermittent effusions. They may develop in young patients with acute knee injuries or in elderly people with degenerative conditions.
The posterior horn of the medial meniscus is broader than the anterior horn, and its anteroposterior dimension is greater than its mediolateral dimension. It aids to the knee’s anterior stability and is therefore more prone to rip in knees with an insufficient ACL. In this set of articles, we provide an in-depth analysis of Medial Meniscectomy and Chondroplasty.
A 76-year-old patient was in our office with complaints of Bl groin pain. Patient was not doing anything specific at the time of the pain happening. Patient has pain walking up hills and sitting and has pain when sitting and has to straighten his leg – he states when he straightens his leg his whole right leg bone hurts and he cannot cross his legs.
He also encountered left knee pain. Patient states feeling a pulling sensation. The pain is mild in intensity and describes the pain as aching. The pain is constant and does not disturb sleep. The problem has been getting worse since it started.
The patient has undergone surgery for prostate, stents (heart), and cortisone shot in leg. Patient has high blood pressure and high cholesterol. Patient is currently taking medication for both high blood pressure and high cholesterol.
Patient has no allergies. Patient is not a smoker. He brought X-ray result and showed no significant degenerative changes. There are no fractures.

Right knee X-ray AP and Lateral with oblique 3 views
He visited after a week for a follow up and presented the results of his MRI and showed mild left hip degenerative change with insertional gluteus Medius tendinosis and partial tearing with mild greater bursitis. Mild RIGHT hip degenerative change. Insertional gluteus minimus tendinosis and partial tearing with mild greater trochanteric bursitis.
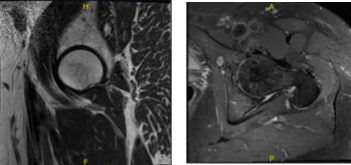
MRI-3T left hip non-contrast
MRI-3T Right hip non-contrast
He got cortisone injection in his right hip at Mather. He feels better after the injection. However, the patient visited again with the complaints of right hip pain. He feels the pain has worsened for the past month. He has a hard time crossing one leg over the other. He describes that pain as burning.
After a week he came back for a follow-up regarding his right knee this time. He underwent cortisone injection to his knee with good results. The patient visited after months and brought x-ray results for his left knee and found no significant degenerative changes and no acute fractures.

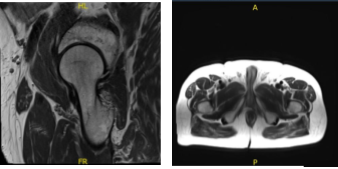
Left knee X-ray AP and Lateral with oblique views
Upon examination of the left knee, the patient is tender to palpation along the medial joint line and has a small effusion. They are nontender to palpation along the medial and lateral facets of the patella. The patient has no discomfort with McMurray’s maneuvers, and the knee is stable.
They have limited range of motion. They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength.
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal.
The patient understands implants may be utilized during this surgery. We have discussed the surgical procedure (Meniscectomy and chondroplasty) as well as the realistic expectations regarding the risks, outcome and post operative protocol.
The patient was taken to the operating room where he was placed on the well-padded operating table. General anesthesia was induced. Tourniquet was applied low on the left thigh. Knee holder was put in place. Esmarch was used to exsanguinate, and the tourniquet was inflated to 300 mmHg.
The left lower extremity was prepped and draped aseptically in the usual fashion. Preoperative antibiotic was already given. A lateral anterior portal was made. Examination of the patellofemoral joint showed stable osteoarthritis grade 2 to grade 3. The scope was moved to the medial compartment when meniscal tear could be seen on the posterior horn.
The medial anterior portal was made using a spine needle. A shaver was entered, and the view was cleaned up. The torn posterior horn medial meniscus and posterior body was taken care of using straight and up biting punches as well as shaver. Now, the scope was moved to the intertrochanteric area where ACL was found to be intact.
The scope was moved well at the lateral tibiofemoral compartment where the lateral meniscus was intact, and the cartilage was in good position without any osteoarthritic changes. The scope was moved back to the patellofemoral joint where the grade 2 to grade 3 arthritis was stable.
There was some fraying, which was cleaned up using the shaver. The scope was entered from the medial portal and reconfirmation of the findings was done.
The knee was irrigated copiously with normal saline. The knee was closed with 4-0 nylon. Depo-Medrol 80 mg and 20 mL of Marcaine was injected into the knee. The patient was extubated and moved to the recovery area in stable condition. Dressing was done using 4 x4, ABD, Webril, and ACE wrap.
We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. Stitches were removed. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
