Case Study: Shoulder Arthroscopic: Rotator Cuff Repair,
Subacromial Decompression and Acromioplasty, Distal
Clavicle Excision, Mini Open Subpectoral Biceps Tenodesis
The acromioplasty, a portion of the shoulder bone, is removed during an operation called an acromioplasty. The treatment is carried out by surgeons to free the impinged rotator cuff tendon, which supports and fortifies the shoulder joint. Subacromial decompression is another name for acromioplasty.
A 36 year-old female patient seen in the office with left shoulder pain due to a mva a few months ago. The patient did not have pain in these body parts before the current injury. She has a history of left shoulder surgery done many years back and she recovered completely and she works as a nurse assistant.
MRIs were reviewed and discussed; Interpretation: There is a full-thickness tear of the distal aspect of the supraspinatus tendon manifest as T2 hyperintense signal within the tendon at its most distal aspect adjacent to the humeral head insertion point.
There is intramuscular fluid within the distal aspect of the supraspinatus muscle proximal to its tendon. There is fluid within the subacromial/subdeltoid bursa below the acromioclavicular joint. There is AC joint hypertrophy.
Examination otherwise demonstrates the osseous structures of the shoulder to be otherwise unremarkable in signal and morphology. Muscular and tendinous structures including remaining portions of the rotator cuff are also felt to remain otherwise unremarkable in signal and morphology.
The glenoid labrum and bicipital tendon appear unremarkable in position and morphology. Impression: Full-thickness tear of the distal aspect of the supraspinatus tendon manifests as T2 hyperintense signal within the tendon at its most distal aspect adjacent to the humeral head insertion point.
Intramuscular fluid within the distal aspect of the supraspinatus muscle proximal to its tendon. Fluid within the subacromial/subdeltoid bursa below the acromioclavicular joint. AC joint hypertrophy.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and I think that is a reasonable option. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to: anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. Ample time was given for questions, of which many were addressed. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post-operative protocol.
We will set this up when it is convenient for the patient. We have instructed them to contact us if there are any questions or concerns between now and their date of surgery.
An MRI was done which showed a tear of the rotator cuff supraspinatus. She was not able to be cleared for months because of her infection, which was controlled with antibiotics. Now, she was brought to the OR.
We discussed treatment options and opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, failure, need for repeat surgery, need for rehabilitation amongst others.
We discussed systemic complications including blood clot, cardiac, pulmonary, and neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was induced. The patient was put in the right lateral position. All the bony prominences were well padded. She was put in place with the use of a beanbag.
She was taped securely to the bag. An axillary roll was used. Left shoulder was prepped and draped aseptically in the usual fashion. A time-out was called. An entry portal was made posteriorly through the soft spot. The arthroscope was inserted.
Superior entry portal was made with the use of a spinal needle. Examination of the shoulder showed tear of the biceps as well as tearing of the labrum. Debridement of the labrum was done with the shaver. It was planned to do a biceps tenodesis and the biceps was cut in the joint and was retracted.
Debridement of the glenohumeral joint was done with a shaver. Arthroscope was inserted into the subacromial space where there was tearing of the rotator cuff in the muscular region. Debridement of the bursa and the tear showed that the tear was difficult to repair.
An acromioplasty was performed with the use of Coblation wand and oval burr. This repair was also performed to take care of the arthritis with use of Coblation wand followed by the #6.0 burr.
Now, my focus was again diverted toward the rotator cuff repair. Partial rotator cuff repair could be achieved with the use of Healicoil #4.75 anchor and suture. Final pictures were taken and saved. The wound was thoroughly irrigated and drained. Closure was done with the use of #4-0 nylon.
Now, the hand was taken out and put in abduction and external rotation. An incision was driven for a subpectoral mini open approach along the anterior fold of axilla. Dissection was done down to the deltopectoral fascia which was cut in the line of incision.
Under the pectoralis, dissection was done to find out the bicipital groove between the lacerated medial tuberosity. Biceps tendon was delivered through the surgical incision. Whipstitch suture was done with the use of FiberLoop and excess biceps tendon was removed.
The biceps tendon was calibrated and with the diamond-tipped Beath pin bicortical followed by a unicortical 7.5-mm drill in the bicipital groove. The suture of the FiberLoop was fitted on to an EndoButton and inserted bicortically through the humerus and tightened.
One of the loops was passed through the tendon and tied over each other to the second point of fixation. Now the thread was passed through the #4 75 bioabsorbable interference screws and the screw was tightened unicortically. Good fixation was achieved at three points.
The wound was thoroughly irrigated and drained. Excess suture was cut. Closure was done with the use of #0 Vicryl, #2-0 Vicryl, and # 3-0 Monocryl. Dressing was done with the use of 4×4, ABD, Webril, and tapes. The patient was put in a shoulder immobilizer, extubated, and moved to recovery in a stable condition.
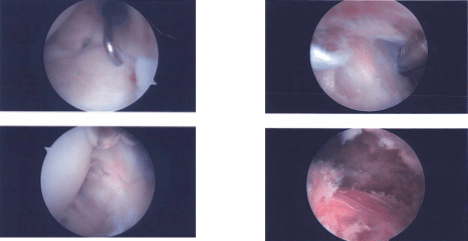
Image documentation
The patient is here today for her postoperative visit, she has no fever, chills, and pain. She is in shoulder immobilizer and sleeps in a recliner. The patient presented with left shoulder pain due to a mva. She has a history of left shoulder surgery done many years back and she recovered completely. She works as a nurse assistant.
After discussing treatment options, we have decided to proceed with a home exercise program for rehabilitation of the shoulder. We removed the stitches during today’s visit. We will continue with ice and elevation of the shoulder to decrease swelling and pain.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications at today’s visit.
I will see them back in three weeks’ time to evaluate their progress. They will call us in the interim if they have any questions or concerns prior to their follow up visit.
After two months, she is not in a shoulder immobilizer. She is working with PT and improving gradually. She has seen Justin Mirza for right wrist pain and is advised surgery. We discussed treatment options including PT, MRI, Injection, surgery and we agreed to go with conservative management for now.
And continue PT, Ice/heat and elevation as a home rehabilitation for the shoulder, taking OTC anti-inflammatory meds and FU after 4 weeks.
After 3 months the patient is here today for her postoperative visit with no fever, chills, and pain. She is not a shoulder immobilizer and is also working with PT and improving gradually. With regular visits in the office, the patient did well after the surgery and continued physical therapy for her shoulder.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
