Case Study: ACL Reconstruction performed
to injured kickball player
A kickball player required six kickball drills to improve his game. It consists of kicking, catching, throwing, pitching, base running and flexibility. All of this requires knee strength that makes his knee prone to injury.
According to the experts, the most common injuries seen in a kickball player are ACL tears, meniscus tears and ankle sprains. In this article we will discuss the surgery performed to a kickball player who was recently involved in a knee injury.
Patient is a 34 year-old male, present with left knee pain due to having knee problems in the past; the patient was playing kickball and the knee buckled. He was seen at Good Sam where crutches were provided.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the aspiration to reduce pain and swelling. After a sterile prep, 5cc of 0.5% Marcaine 125cc of blood was aspirated from into the left knee and 5cc of 0.5% Marcaine was injected.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
Patient also mentioned that he got surgery on the same last month for his medial and lateral meniscus, and wanted to completely ease the pain in order for him to get back to playing kickball.
An MRI was done which showed tears of the medial and lateral meniscus as well as the ACL. We discussed treatment options and opted for surgical management at that time. He was taken for arthroscopic surgery a month back when repair of the meniscus root and the lateral meniscus was performed.
ACL repair versus reconstruction was deferred as there was no time left from the tourniquet. I met the patient in the postop period and started rehabilitation. He has been doing well. We discussed options for management of the ACL tear.
He opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, failure and need for repeat surgery, need for rehabilitation, knee stiffness, systemic complications including blood clots, cardiac, pulmonary, neurological complications among others. The patient understood and signed an informed consent.
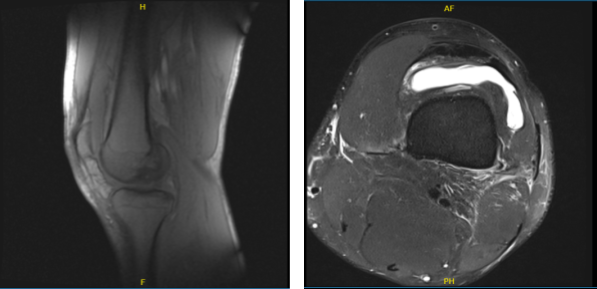
MRI of the left knee
The patient was taken to the operating room where general anesthesia was induced. Left knee range of motion was 0 to 90 degrees. Manipulation of the knee was performed to reach a range of motion of about 120 degrees. Preop antibiotic was given.
Tourniquet was applied. Left knee was prepped and draped aseptically in the usual fashion. Exsanguination was done and tourniquet was elevated. One gram of tranexamic acid was also given. A time-out was called.
An entry portal was made. An arthroscope was entered and examination of the medial meniscus was performed. The meniscus root was found to be healing well and intact. Examination of the lateral meniscus showed the medial margin of the lateral meniscus which was debrided.
There were a couple of loose sutures that were removed. The rest of the meniscus was healing well. Examination of the ACL showed a stump on the ACL, which was shortened. It could not be reached. We decided to do a reconstruction.
At this time, the arthroscope was removed and quad tendon harvest was planned. A suprapatellar incision was given. The tissue was cut in the line of incision. The paratenon was reached and it was cut in line of Incision high up into quadriceps.
The quadriceps tendon was exposed till the patella. After dissection and cleaning, a 10 mm blade was used inside the tendon on the medial side. Further tendon exposure was done with #15 blade.
A 10-mm wide tendon was stripped with the use of a cookie cutter to a length of 17 mm. The graft was prepped on the back table by the PA with the use of FiberTaks. I also helped in the preparation of the graft.
In the meantime, the graft was prepped and then measured to be 9.5 mm. The ends were also prepped. The graft was wrapped in a vancomycin-wet Ray-Tec. In the meantime, the arthroscopic debridement of the ACL stump was performed.
Preparation of the superior entry portal was done. Once the graft was prepped, the entry portal on the lateral condyle was prepped with the use of ACL to the left. Separate incision was given laterally and sleeve was inserted on to the bone. A 9.5 mm FlipCutter was used and inserted in the desired position.
The cutter was flipped and a 30 mm tunnel was made. The FlipCutter was removed. FiberStick was used to hold the portal. Now, the tibial tunnel was prepared using a tibial tunnel to the left. FlipCutter was again used and the 30-mm tunnel was again made. FiberStick was again used.
Once this was done, PassPort was introduced. the bone debris. The femoral side of the ACL graft was loaded on to the femoral FiberStick and procured. The button was flipped. The was tightened to secure the graft into was flipped over the surface of the tibia were tightened again to find the graft in a stable were again tightened completely.
The knee was thoroughly irrigated and drained. The closure was done in layers using nylon for the portals and #0 Vicryl, #2-0 Vicryl and #3-0 Monocryl for the posterolateral incision. Dressing was done with the use of Xeroform, 4×8, ABD, Webril, and ACE wrap. Knee immobilizer was applied and locked in extension.
After a week the patient came back to the office for post-operative checkup. Post Operative Exam: General Appearance: swelling and tenderness and wound clean and dry, no warmth, appropriate range of motion, and neurovascular intact. He is here for his postoperative visit, no X Rays were needed.
Patient got well on his surgery. By following the RICE Therapy (Rest, Ice, Compression and Elevation) and continuous follow up, patients tolerated it. For full recovery we decided to start physical therapy and he will continue to see me until he recovers and is able to do his normal routine.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
