Case Study: Knee Arthroscopy with Medial Meniscectomy
in a 60 year-old female
A meniscectomy (meniscus removal) is a surgical treatment that removes all or part of the cartilage around your knee (called the meniscus). If you tear your meniscus, your doctor may recommend full or partial meniscus removal.
A 60 year-old female patient seen in the office with complaints of left knee, left hip, back, right knee. She had a fall at the place she lived in which she injured her head and had injuries to left hip, both knees and back. She also got injured in a car in which she was sitting.
This accident exaggerated her pain in both knees, left hip, low back and neck. Since then, she has been walking with 2 canes. She had a history of OM in spine in the past years and has been using cane off and on since many years.
An MRI was reviewed and discussed by the doctor; Left Thigh MRI, the Bones T1 marrow signal intensity is maintained within without evidence for aggressive osseous lesion or osteonecrosis. No acute fracture is present. There is no marrow or periosseous edema.
Please note that this study was not tailored to evaluate for internal derangement of the Joints. Nevertheless, no significant joint effusions are present. There is an oblique tear in the posterior horn of the medial meniscus. The Muscles/Tendons has no full-thickness tendon tear or tenosynovitis is appreciated.
There is no disproportionate muscle atrophy. No acute muscle tear or denervation-related edema is present. There is no peri muscular fluid. The neurovascular structures demonstrate normal course.
The subcutaneous tissues are within normal limits. Oblique tear in the posterior horn of the medial meniscus. No fractures. No muscle tear or muscle edema in the thigh.
In left hip MRI, Bone and Joint there is severe joint space narrowing the left hip joint with bone-on-bone contact. There is subchondral bone marrow edema subchondral cyst in the lateral acetabulum and lateral aspect of the femoral head with bone marrow edema extending into the femoral neck and intertrochanteric fossa.
There is flattening of the femoral head. There is extensive full-thickness cartilage loss. There is a moderate left hip joint effusion with synovitis. There is diffuse tearing of the labrum. The Tendons/Muscles have visualized tensor fascia lata, rectus femoris, hamstring tendons and iliopsoas intact.
No iliopsoas bursitis is noted. The gluteus Medius and minimus insertions are intact. No trochanteric bursitis is noted. The ischiofemoral interspace and quadratus femoris muscles are intact.
The piriformis muscles and the common rectus abdominis, and adductor aponeurosis are intact. The visualized sciatic nerve is intact. There is marked scoliosis.
The nerves have a fat plane surrounding the sciatic nerve. In Pelvis and Contralateral Hip: The pubic symphysis is intact. There is marked osteoarthritis in the right hip joint. The visualized pelvic visceral structures appear normal. No enlarged lymphadenopathy. No free fluid in the pelvis.
The periarticular subcutaneous tissues are unremarkable. It has a severe osteoarthritis in the left hip joint with associated subchondral bone marrow edema in the femoral head and neck and flattening of the femoral head. Diffuse tearing labrum. Moderate left hip joint effusion.
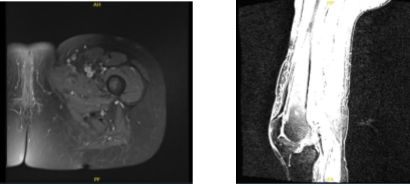
MRI Left thigh non-contrast
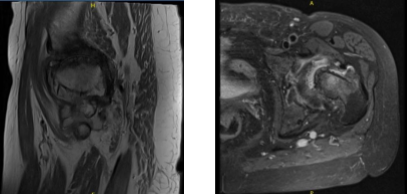
MRI Left hip non-contrast
Upon the examination, we discussed the treatment options for the patient’s diagnosis, which included: non-surgical and surgical options. We discussed risks and benefits including infection, bleeding, nonhealing, need for repeat surgery, rehabilitation, injury to adjacent nerves and vessels.
We also discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and expressed a desire to proceed with surgery and signed the informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion.
Preop antibiotic was given. Tourniquet was inflated. Time-out was called. Lateral anterior portal was made for the arthroscope and the examination of the knee was done. An arthroscope was inserted.
A medial entry portal was made under arthroscopic visualization and was performed using a spinal needle. Examination of the medial tibiofemoral compartment showed fraying anterior of the medial of the lateral margin of the medial meniscus. There was no tear along the body of the posterior horn. Debridement of the medial meniscus was done using biters and shavers.
Examination of the cartilage showed injected cartilage of the medial femoral condyle. Examination of the intercondylar notch showed intact ACL. Examination of the lateral compartment showed intact cartilage. There was a tear of the mid body of the lateral meniscus, which was debrided with the use of the shaver.
Examination of the medial femoral compartment showed grade 1 to grade 2 cartilage loss of the lateral facet of the patella. Debridement was done with the use of a shaver.
Final pictures were taken and saved. The knee was thoroughly irrigated and drained. Closure was done using # 3-0 nylon. The 40 mg of Depo-Medrol mixed with 30 cc of 0.5% Naropin was injected into the knee. Dressing was done using Adaptic, 4x4s, ABD, Webril and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
After one week the patient is seen in the office for post operative visits, she denies fever, chills. The pain control is getting better. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during visits. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications.
After two weeks the patient visits the office for follow up checkup, she denies fever, chills. The pain control is getting better. However, she has left hip pain which has been bothering her.
We agreed to go with conservative management for now and she sees a pain physician. With the continued follow up checkup the patient showed progress from time to time she visits the office. She gets well after the surgery and with the help of continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
