Case Study: Knee Arthroscopy: Medial Meniscectomy
and Chondroplasty in a 53-year-old Female
Chondroplasty is a procedure that involves smoothing degenerative cartilage and reducing unstable cartilage flaps in order to stabilize and treat chondral lesions. Trimming unstable flaps of a torn meniscus to create a stable remnant meniscus is what partial meniscectomy entails.
A 53 year-old female went to the office with her X-ray and complained of right knee pain for about weeks and she does not remember if it is from fall or injury, she has not gained weight, fever, chills. Upon the physical and X-ray examinations result, Sunrise patella, AP and lateral.
Distal femur, patella, proximal tibia and proximal fibula demonstrate intact cortical margins with no acute fracture. There is a suggestion for a healed fracture proximal shaft right fibula. There is mild narrowing of the medial joint compartment with slight osteophyte formation
There is spurring from the superior pole of patellar anteriorly. A joint effusion is present There is no radiographic evidence of soft tissue swelling. There are mild osteoarthritic degenerative changes. A joint effusion is present. There are no fractures.

Right knee X-ray AP and Lateral
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the aspiration to reduce pain and swelling. After a sterile prep, 3cc of 1% Lidocaine infiltration, 60 cc of blood collection was aspirated from into the right knee joint and 60mg of ketorolac was injected.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail. Used Ice, Elevation and OTC anti inflammatory meds for pain if tolerated.
Then, after 2 days the patient goes back to the office complaining that her pain is getting better but she is still limping and not able to work. The doctor instructed her to continue with the Ice, Elevation and OTC anti-inflammatory meds for pain if tolerated. And the patient was instructed to contact the office if there were any questions or concerns and do an MRI prior to their follow up appointment.
MRI reviewed and discussed by the doctor; Intra-articular body seen within the suprapatellar bursa measuring 10.2 mm. soft tissue edema seen within the superficial soft tissues surrounding the right knee.
Large effusion has no popliteal cyst is visualized and no evidence of stress injury, fracture, osteonecrosis or osseous neoplasm. No arthritic changes are visualized, the medial meniscus is unremarkable in MR appearance, without evidence of degeneration or tear.
The lateral meniscus is unremarkable in MR appearance, without evidence of degeneration or tear. The ACL, PCL, collateral ligaments, iliotibial band, fibular collateral ligament and biceps femoris tendon, popliteus muscle-tendon unit are all unremarkable.
The patella is inferiorly displaced with wavy patellar tendon and associated tear of the medial quadriceps. The impression of this is the Medial quadriceps tear, Cruciate ligaments and menisci are intact, the Intra-articular body in the superior patella bursa measuring 10.2 mm. and has Effusion.
MRI was done, it showed osteoarthritic changes and which showed a loose body in the suprapatellar pouch. We discussed treatment options and the patient opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, inability to resolve the pain and swelling, inability to find the loose body, knee rehabilitation, blood clots, cardiac, pulmonary, neurologic complications. The patient understood and signed an informed consent.
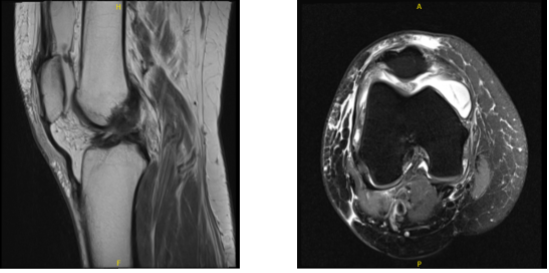
MRI-3T Right knee non-contrast
The patient was taken to the operating room where She was placed on the well-padded operating table. General anesthesia was induced. Right lower extremity was prepped and draped aseptically in the usual fashion. Time-out was called. Preoperative antibiotic was given. tourniquet was elevated.
A lateral arthroscopic portal was made for arthroscopy insertion. Arthroscope was inserted. A Medical portal was made with the help of a spinal needle. Examination of the patellofemoral joint showed no loose body there. There was a lot of synovitis.
There was grade 1 to grade 2 osteoarthritic changes of the patella as well as trochlea. The medial gutter showed no loose body. Medial tibiofemoral compartment showed partial tearing of the lateral and posterior edge of the anterior horn of the medial meniscus.
Examination of the intercondylar notch showed again synovitis with ACL. Lateral examination of the tibiofemoral compartment showed infected lateral meniscus and no osteoarthritic changes on the lateral compartment. Shaver was used to do chondroplasty of the patella as well as trochlea and the medial femoral condyle.
Backbiters to the left and right were used to do meniscectomy of the anterior Hom of the medial meniscus. Lateral was done. Total synovectomy was performed with the use of a shaver. Synovectomy was done in the medial and lateral gutters as well as suprapatellar pouch.
Synovectomy was also done from the intercondylar notch. Examination of the left gutter also showed no loose body. The scope was switched to a medical portal also to examine and no loose body would be found.
Finally, the scope was inserted into the posterior compartment and a 70-degree scope was taken to examine the posterior compartment and no loose body could be found there too.
The knee was attempted a number of times to dislocate the loose body from its position but thorough examination ended up negative for any loose body. Fluoroscopy was also used to examine and see if a loose body could be traced on x-ray but could not be found. Decision was taken not to search any more.
The knee was thoroughly irrigated and drained. Final picture was saved. Closure was done using #3-0 Nylon. Then, 9 cc of Marcaine 0.5% mixed with 40 mg Depo-Medrol was injected into the knee. Dressing was done using 4 x 4, ABD, Webril and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
After a week, the patient seen by the doctor for her post operative visits is using a single crutch, still limited in motion, swelling and tenderness. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We removed the stitches during visits. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate their progress.
After three weeks the patient was seen at the office for her postoperative visit, no x-rays were needed. She is not using crutches, though her pain has improved but not resolved. Discussing the treatment options, we agreed to go with conservative management for now.
Physical therapy to be started, continued with ice and elevation of the knee to decrease swelling and pain and OTC anti-inflammatory meds. Another week has passed, the patient visits the office for her post operative consultation, she is not using crutches, her pain has improved but not resolved.
She is still limping. We agreed to continue the medical treatments and she will be back to the office after a month.
After two months the patient visits the office for her follow up checkup, the patient is not using crutches, her pain has improved and she is not limping. With the continued follow up checkup the patient showed progress from time to time she visits the office.
She gets well after the surgery and with the help of continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
