Case Study: Knee Arthroscopy: Lateral Meniscectomy
Chondroplasty in a 39-year-old male
The surgical procedure known as knee arthroscopy may be utilized to identify and address knee joint issues. An operation called a meniscectomy is performed to repair a meniscus that has been injured. In addition to this, lateral meniscus serves as a shock absorber and helps the knee to become steady.
It makes and keeps the joint lubricated which also normalizes the movement of the joint to avoid knee hyperextension. In this set of articles, we provide an in-depth analysis of Lateral Meniscectomy Chondroplasty.
The meniscus is a stretchy structure that can easily tear if twisted during an abnormal motion which will result in being torn or ripped. A lateral tear can cause a person to have restricted movement in their leg and make it hard to extend it. However, with meniscus transplant surgery, damages to the lateral meniscus can be corrected.
A 39-year-old patient visited our office, with complaints regarding left knee pain for almost a month now in which he got while working at Long Island Rail Road, where he usually used his lower extremity most of the time during work hours.
The pain is moderate and in constant intensity which is also associated with swelling. The pain is not associated with bruising, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, or limping, hand function difficulty.
The problem has been getting worse since it started. However, stairs make the symptoms worse but with the help of rest, ice, and electric machines makes the symptoms better. Patient has had right knee surgery (ACL recon and patellar microfracture) in 2008-9. Patient is taking ibuprofen but is allergic to penicillin.
Upon examination of the left knee, the patient has mild effusion. Positive lateral joint line tenderness. There is no pain with manipulation of the patella. There is no crepitation with passive or active range of motion. There is no medial joint tenderness. McMurray’s maneuver is positive for lateral joint line tenderness.
Collateral ligaments are intact. Lachman’s test negative. Anterior drawer and posterior drawer negative. There is no soft tissue swelling distally. Neurovascular examination is intact.
On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength.
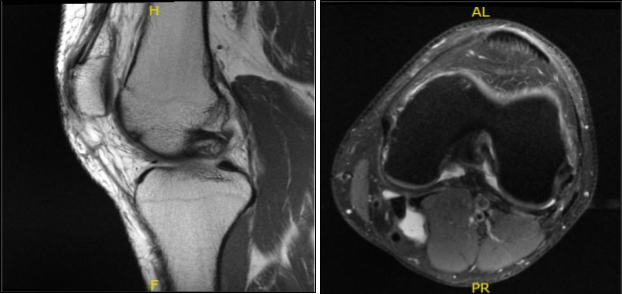
MRI results were presented today and showed lateral meniscal tear. Mild partial-thickness cartilage loss along the central trochlear groove and in the lateral compartment. Trace left knee joint effusion and small Baker’s cyst.
MRI-3T Left Knee Non-contrast
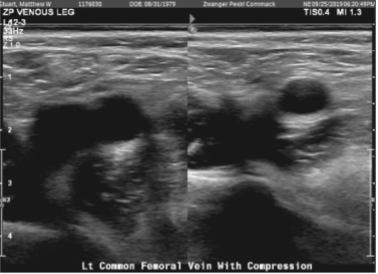
Doppler venous left lower extremity
There are findings consistent with deep vein thrombosis of the left leg. Specifically, there are findings consistent with deep vein thrombosis involving the visualized posterior tibial venous system. The appearance is consistent with acute deep vein thrombosis.
We discussed treatment options and the patient opted for surgical management and discussed the risks, benefits, complications of surgery including infection, bleeding, injury to adjacent nerves and vessels, retear, need for repeat surgery following possibility of repair and need for rehabilitation following the repair. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was Induced. The left lower extremity was put in a tourniquet and prepped and draped in an aseptic usual manner. Preoperative antibiotic was given. Tourniquet was elevated. A lateral entry portal was made and the scope was introduced.
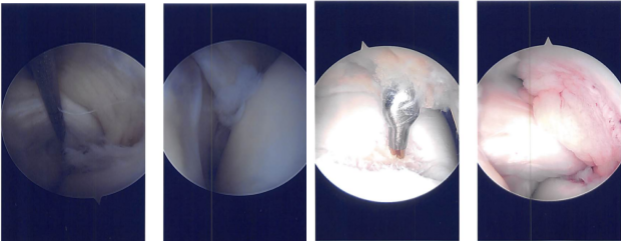
The patellofemoral joint was checked. The posterior surface of the patella was pristine, but there was a large grade 3 to grade 4 osteochondral lesion in the trochlea.
Lateral meniscus showed a tear in the posterior body of the lateral meniscus vertical radially oriented up to the periphery. There was a grade 1 to grade 2 osteochondral lesion on the lateral femoral condyle also.
Intraoperative Arthroscopy Images
A medial entry portal was made with direct access to the lateral meniscus. A shaver and upbiters were Introduced and the meniscectomy was performed as the meniscus was not amenable to repair. A stable margins were reached. The chondroplasty of the lateral femoral condyle was done.
The chondroplasty of the trochlea was also done and considering it to be a grade 4 lesion. A microfracture was performed. Fat globules could be seen coming out. Dressing was done. The patient was moved to the holding area from the postoperative care unit in a stable condition after extubation.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.