Case Study: Tendo-Achilles Repair of the Left ankle
in a 46 year-old patient
An incision in the back of the calf is created during the procedure. The tendon will be stitched back together by the surgeon if it has ruptured. Depending on how deteriorated the tendon is, the surgeon may cut away the degenerated portion and patch up the remaining tendon.
An abrupt rise in the tension on your achilles tendon frequently results in ruptures. Increased engagement in sports, particularly those involving leaping, at a higher level is one frequent example.
You could hear a pop, then feel an acute, severe pain in the back of your ankle and lower leg that will probably make it difficult for you to walk normally if your achilles tendon ruptures. The rupture is frequently repaired surgically. But for a lot of people, nonsurgical treatment is just as effective.
A 46 year-old patient complaining of left ankle pain. It started when he was playing basketball. He landed on his left ankle and twisted it. Since then, it has been painful and swollen. Varies in quality and severity. It is causing him to limp. Denies pain elsewhere. Denies previous injury.
MRI was reviewed that showed full-thickness achilles tendon tear at the myotendinous junction 6 cm from the calcaneal insertion with a 4 cm gap retracted tendon stumps. Complete tear of the anterior talofibular ligament and calcaneofibular ligament. Diffuse lateral and posterior soft tissue edema.
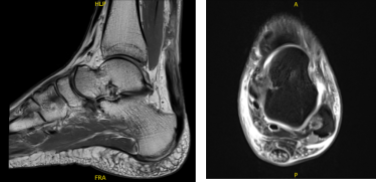
MRI Left ankle non-contrast
We discussed treatment options and we opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to the adjacent nerves and vessels, numbness, need for splint and boot in the future, need for rehabilitation, chances of rerupture and re-repair or reconstruction among others.
We also discussed systemic complications including blood clot, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where general anesthesia was induced. The patient was flipped prone onto the operating table. Bumps were put on the chest and on the site with abdomen free.
All the bony prominences were well secured. A tourniquet was applied over the left thigh. Left lower leg was prepped and draped aseptically in the usual fashion. The tourniquet was elevated.
A medical incision was done. About 55 minutes of tourniquet time was used. With sharp dissection, the paratenon the incision was just above the defect and about a centimeter distal to it.
After the paratenon was opened, the tendon could be seen torn completely. Debridement and irrigation of the tendon ends were done. It was decided to pass Krackow sutures into the proximal stump; 2-mm FiberTape was used and Krackow sutures were passed x2 with four tails appearing at the distal end of the proximal segment.
It was decided to fix it into calcaneus with the use of SwiveLocks. Two stab incisions were given on either side of the calcaneal tuberosity on either side of the tendo-Achilles insertions. A Banana Lasso was passed sequentially from one side and then the other along the distal portion of the tendo-Achilles and the two ends were far from either side and procured distally.
Drilling and tapping was done on either side of the calcaneus tuberosity at 45-45 degree angles. A 4.75 Swivelock was used on either side to dunk the sutures into the calcaneal tuberosity under tension with the foot in plantar flexion. A nice opposition of the tendo-Achilles tendon ends could be reached.
Final repair was checked and found to be satisfactory. Wound was thoroughly irrigated and drained. Closure was done in layers with the paratenon closed with #0 Vicryl, followed by #2-0 Vicryl for subcu and #3-0 Monocryl for the skin. The stab incisions were also closed with the use of Monocryl.
Dressing was done with the use of Xeroform, 4 x 4s, ABD, Webril. Posterior plaster splint was applied with the ankle in 20 degrees plantar flexion and Ace wrap was applied. The patient was flipped supine and extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the ankle. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his ankle.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
