Case Study: Knee Arthroscopy: Patellofemoral Chondroplasty
and Partial Medial Meniscectomy for 28 year-old male athlete
Knee arthroscopy is an important diagnostic and treatment technique for knee illness. Meniscus removal, loose body removal, chondroplasty, microfractures, irrigation and debridement, and tendon repair are some of the reasons. We present a thorough analysis of patellofemoral chondroplasty and partial resection of the medial meniscus in this case.
Chondroplasty is a surgical procedure that involves flattening degenerating cartilage and trimming unstable cartilage flaps in order to strengthen and cure cartilage lesions. The unstable flaps of the torn meniscus are removed during partial meniscus removal, leaving a secure residual meniscus.
A 28-year-old male patient complained of a left knee injury sustained while playing soccer. He experienced moderate pain and swelling and had trouble carrying his weight. Upon examination of the left knee, the patient has moderate effusion.
There is complete freedom of knee joint movement. There is no pain in manipulating the patella. There is no crepitation in passive or active range of motion. There is no medial joint tenderness.
Positive sensitivity of the lateral joint line. McMurray’s maneuver is positive for lateral joint line sensitivity. The lateral ligament is intact. Lachman test was performed and no strong evidence of an existing anterior cruciate ligament (ACL) tear.
There is no distal soft tissue swelling. The neurovascular examination remains unchanged. Examining the contralateral limb, the patient does not palpate and has excellent range of motion, stability, and strength.
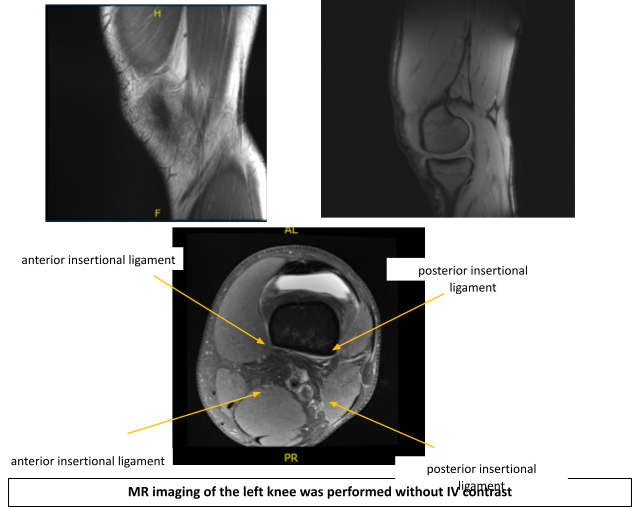
An MRI was performed. There is a complex tear of the lateral meniscus with displacement of the majority of the posterior horn and body-posterior junction displaced anteromedially, immediately posterior to the anterior horn.
There is intra-meniscal cyst formation within the displaced meniscus as well as within the native anterior horn with a cluster of parameniscal cyst seen anteriorly measuring up to 1.2 x 1.4 x 1.5 cm (craniocaudal x anteroposterior x transverse dimension). There is full-thickness cartilage loss overlying the central weight bearing aspect of the lateral femoral condyle spanning approximately 1.4 x 0.5 cm with a nondisplaced delamination flap medially.
We discussed conservative and surgical management of her current pain pattern. The patient understands that arthroscopy does not guarantee all pain relief. Patients understand that they are at risk of infection, postoperative pain, numbness, tingling, stiffness, DVT, PE, MI, CVA, and other unforeseen events.
Patients also understand that there is usually a long rehabilitation process after a surgical procedure. The patient understands that implants and sutures may be used during this procedure.
Patients also understand the associated general anesthesia risks and want to proceed selectively. Patients are aware of the limitations and risks and want to proceed with elective arthroscopic surgery.
Operation started with inducing general anesthesia. A tourniquet was applied along the mid-thigh and Esmarch was applied and the pressure was elevated.
The left lower extremity was prepped. A lateral arthroscopic portal was made through which the scope was entered. Patellofemoral joint was examined and found to be normal.
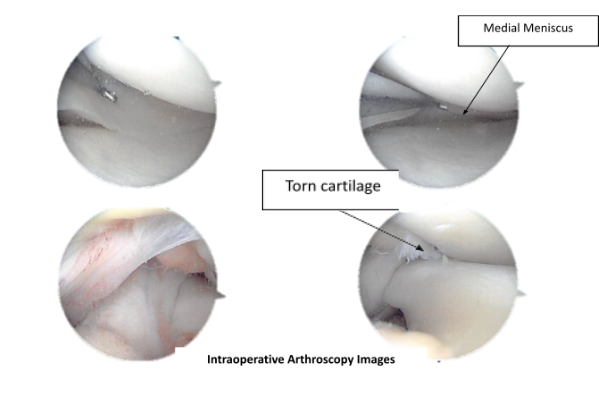
Medial compartment was examined and there was grade 1 fraying of the articular cartilage of the medial tibial condyle. The loose cartilage flap was shaved.
The lateral meniscus was found to be extruding into the intercondylar region. Probe was introduced and tear was examined and found to be around the mid-substance with fraying of the meniscal edges.
The tear was not found to be repairable. The torn meniscus was removed using punches and shaver. The anterior horn had a meniscal cyst, which was decompressed using the shaver.
Extensive debridement of the meniscus led to a removal of 60% to 70% of the meniscus with retention of peripheral rim, part of anterior horn and anterior body and posterior horn.
The damage chondral was found to be in the posterolateral part of the lateral femoral condyle which measured to be more than 20mm x 5 mm. It was OA grade 3 to grade 4 chondral damage. The chondroplasty was performed, the damage was enough for the need of secondary reconstructive procedure for the cartilage.
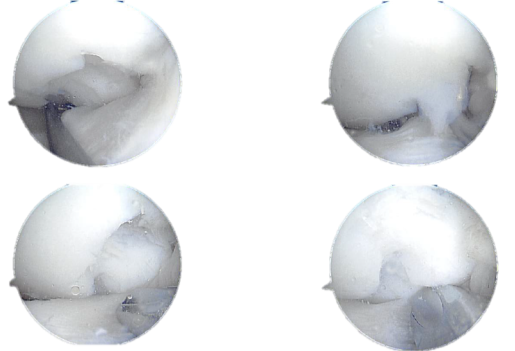
Arthroscopic view tear of the lateral meniscus posterior horn
Final arthroscopic pictures were taken and saved. The knee was washed with saline and scope was removed. The incision was cleansed with nylon 3-0 and dressing was done with Adaptic, 4 x 4 and BD followed by Webril and Ace wrap. The tourniquet was removed. The count was complete at the end of the procedure. The patient was extubated and moved to the stretcher and into the postoperative care unit.
After 1 week, the patient showed signs of improvement in discomfort and swelling, walking with a limp and moving with assistive devices. Deny fever, chills, or reinjury. The incision has healed well 2 weeks after surgery, with no evidence of drainage, erythema, or warmth.
Complete freedom of movement without pain. I decided to combine formal physical therapy with a home exercise program to rehabilitate my knee. The patient returned to the clinic every 3-4 weeks. The patient recovered well from surgery and continued physical rehabilitation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
