Case Study: Medial and Lateral Meniscectomy with
Medial Meniscus Root Repair and Abrasion Chondroplasty
performed to 63 year-old female patient
Patient seen in the office with complaints of having left knee pain. She is 63 years-old and currently working at the bank. She states she leaned entirely on her knee and possibly twisted the knee and heard a crunch and that’s when the pain started and she had toe fractures recently.
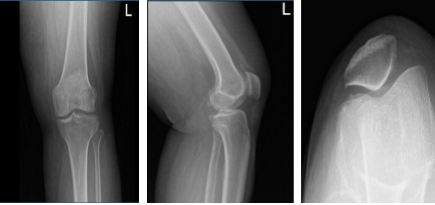
She had an X-ray result, we reviewed and discussed it. X-ray results showed normal radiographs considering her age, severity of pain, and inability to do activities of daily living and work, that’s the time we agreed to go with 3 tesla MRI of left knee to see the reason behind it. By this time, she will take tramadol until her next visit with an MRI result.
Left knee x-ray complete with patella
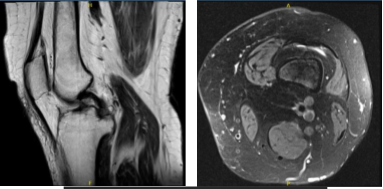
Patient MRI showed significant results. Impression as follows: Vertically oriented tear of the posterior horn medial meniscus extending to the posterior root attachment of the junction of the inner and central thirds.
Shallow fraying of the undersurface of the medial meniscal body. Mild MCL sprain. Mild to moderate chondromalacia patella as well as cartilage loss at the periphery of the lateral trochlea. Joint effusion and thickened medial parapatellar plica.
MRI-3T Left knee non-contrast
We discussed treatment options and the patient opted for surgical management. We discussed risks and benefits including infection, bleeding, nonhealing, injury to adjacent nerves and vessels, need for repeat surgery, need for rehabilitation, and possible need for total knee replacement in the future.
Systemic complications including blood clots, cardiac, neurological, pulmonary complications including death. The patient understood and signed an informed consent.The patient was taken to the operating room where she was placed on a well-padded operating table.
General anesthesia was induced. The left lower extremity was prepped and draped aseptically in the usual fashion. Preoperative antibiotics were given. Time-out was called. Tourniquet was inflated over the left lower extremity. Tourniquet time was 75 minutes for the surgery.
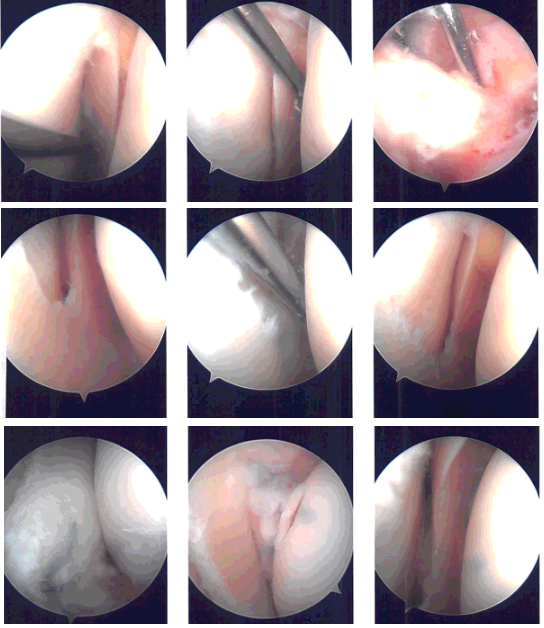
Lateral entry portal was made. Arthroscope was introduced. There were grade 2 to grade 3 osteoarthritic changes on the posterior surface of the patella on the lateral facet. There were loose cartilage fragments in the medial gutter. Examination of the medial compartment showed medial meniscus tear.
The medical entry portal was made using a spinal needle. A shaver was used to clear the joint as well as the meniscus. Biters were used sequentially to do the medial meniscectomy in the mid portion of the body.
The posterior root of the meniscus was found to be loose and on further examination, it was found that it was torn from the whole knee attachment. A decision was done to do a repair of the meniscal root. Examination of the Intercondylar notch showed the ACL was intact.
Examination of the lateral tibiofemoral compartment showed fraying and tearing of the medial edge of the lateral meniscus, which was cleaned using the biter as well as the shaver. Examination of the patellofemoral compartment showed grade 3 to grade 4 osteoarthritic changes of the lateral trochlea as well as the lateral facet of the patella.
Chondroplasty was performed. The scope was entered from the medical portal to re-confirm the findings. Again, the scope was entered from the lateral portal and repair for the medial meniscus root was planned.
The Arthrex jig was used to make an entry portal from the medial tibial condyle into the posterior plateau. The FlipCutter was used to make a depression for the root to insert and abrade the bone intraarticularly. Knee Scorpion was used to pass two FiberLinks.
The FiberLinks were sutured through the canal using suture lasso. The sutures were put in tension and fixed to the tibia using SwiveLock #4.75. Final pictures were again taken and saved.
The knee was thoroughly irrigated. Microfracture of intertrochlear notch was done using the chondral pick set. Fat pad could be seen coming out of the microfracture. The knee was irrigated and drained. The knee was closed using # 4-0 nylon. A 30 cc of Naropin was injected into the knee.
Dressing was done using Adaptic, 4×4, Webril, and Ace wrap. Knee immobilizer was applied. The patient was extubated and moved to recovery in a stable condition.
Intraoperative Arthroscopy Images
After a week the patient was required to return to the office to check her condition. Post Operative Exam: General Appearance: swelling and tenderness and wound clean and dry, no warmth, appropriate range of motion, and neurovascular intact.
Has pain, which has been improving and denied fever and chills and has difficulty sleeping. Patient showed progress from time to time when she visited our office. She gets well after the surgery and with the help of continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.