Case Study: Management of 55-year-old Female with
Medial Meniscus Tear of the Left Knee
A 55-year-old female patient presented to us with complaints of left knee pain and a snapping/popping sensation. The patient reported injuring her left knee while playing with her grandson. She reported a subsequent swelling in the left knee which subsided after a few days. During the acute injury, she did not seek medical attention and used NSAIDs for pain relief.
A month after the initial injury she reported worsening pain and stiffness in the left knee. She describes the pain as sharp which is located in the inner surface of the left knee. The pain is non-radiating and gets worse on walking or bearing weight. The patient reports occasional use of NSAIDs and Tramadol secondary to pain. She attended physical therapy but had minimum relief.
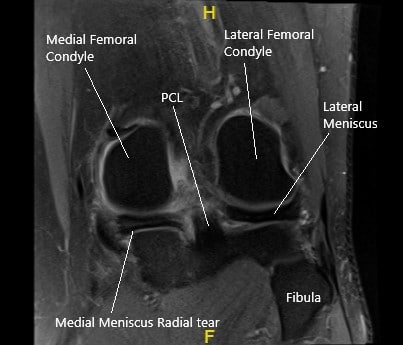
MRI of the left knee in the coronal section showing the torn medial meniscus.
The patient’s past medical history is unremarkable and she denies the use of any illicit drugs. The patient is a former smoker with a history of 15 pack years. The patient is currently not working. She walks with an antalgic gait and uses a cane for ambulation.
On physical examination, there is tenderness to palpation on the medial joint line and a positive McMurray’s test. The rest of the examination and the examination of the right knee is normal. The neurovascular examination of both the lower and upper extremities is normal.
MRI of the left knee suggested a tear of the posterior horn medial meniscus, notably with a radial component within the inner third, with meniscal extrusion into the medial gutter. There is tri-compartmental arthrosis, most pronounced over the patellofemoral compartment. Tendinosis of the extensor mechanism. Semimembranosus insertional tendinosis.
Various treatment options were discussed with the patient at length and the patient opted for surgical management. The risks and benefits of surgery including infection, bleeding, nonhealing, need for repair, inability to heal, injury to adjacent nerves and vessels, recurrent symptoms, knee arthritis, knee pain, need for rehabilitation among others were discussed at length with the patient. The patient understood and signed the informed consent.
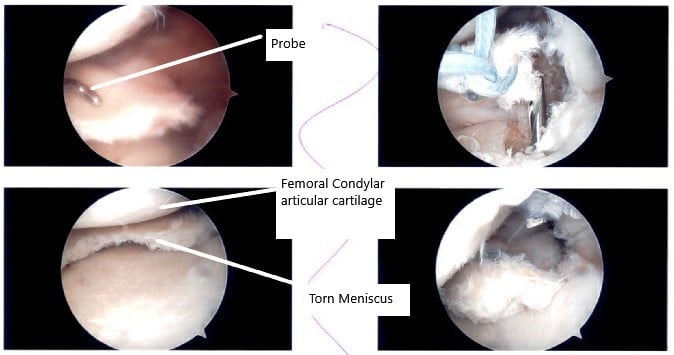
Intraoperative arthroscopic images showing the meniscus tear.
PREOPERATIVE DIAGNOSIS: Medial meniscus tear of the posterior horn, left knee.
POSTOPERATIVE DIAGNOSES:
- Medial meniscus tear of the posterior horn, left knee.
- Posterior root rupture of the medial meniscus, left knee.
- Grade 3 to grade 3 arthritic changes of the trochlea and the patella of the left knee.
OPERATION:
- Partial medial meniscectomy, left knee.
- Posterior root repair of the left knee medial meniscus
- Chondroplasty of the patella and the trochlea of the left knee.
- Intraarticular injection of Naropin.
DESCRIPTION OF PROCEDURE: The patient was taken to the operating room where general anesthesia was induced. He was put on a well-padded table. The left lower extremity was prepped and draped aseptically after application of a low thigh tourniquet. A time-out was called. Preoperative antibiotics were already given.
A lateral working portal was made and the arthroscope was introduced. The patellofemoral joint showed grade 2 to grade 3 arthritis on the inferior surface of the patella as well as trochlea. A medial entry portal was made using a spinal needle. A shaver was introduced followed by scope.
The scope showed that there was a tear of the lateral inner margin of the medial meniscus. The tear was debrided. After debridement of tear, it was found that the meniscal root was loosely attached. It was immediately detachable.
A decision was made to repair the meniscal root. The scope was entered into the intercondylar area where it was found to be intact. We thus moved to the lateral compartment where minimal fraying of the inner margin of the lateral meniscus was found.
The knee scope was entered into the patellofemoral compartment where chondroplasty of the posterior surface of the patella and the inferolateral aspect as well as the trochlea was performed. The knee scope was again introduced into the medial compartment where debridement of the meniscus was performed.
A #5 FiberWire suture was passed twice through the meniscal root using Firstpass and PDS sutures. They were looped onto themselves. An ACL rim was chosen to mark the insertion of the roots. A separate incision was made on the medial shin.
A guidewire was passed into the tibia and out into the intraarticular portion near the root of the medial meniscus in a satisfactory position. The guidewire was removed and a Hewson Suture Passer was passed. The sutures were passed through the suture passer and retrieved out of the shin incision. The sutures were tied over in the bottom. The final pictures were taken and saved.
The knee was thoroughly lavaged and closure was performed using #3-0 nylon. Then, 20 ccs of 0.5% Naropin was introduced into the knee joint. Tourniquet was removed. The dressing was done. The patient was moved to the recovery unit in stable condition. The patient’s left knee was put in an immobilizer.
The patient’s husband was informed about the surgery and instructed about the care management of the knee including ambulating with crutches with 50% partial weight-bearing with the knee in extension at all times. The immobilizer can be loosened while resting and sleeping.
The patient had an excellent recovery post-op and reports minimal pain while participating in physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
