Lumbar Spine Surgery
Patients who have failed conservative treatment for their lumbar spine pathology or patients to sudden onset or worsening of their neurological symptoms, may need to undergo lumbar spine surgery.
The surgery is usually done for the back and nerve roots are decompressed. The surgery may vary from discectomy to laminectomy to fusion surgery. Discectomy can be done with the use of endoscope or microscope or in an open fashion depending on patient’s disease and characteristics. Patients who have stable spine and have compression of the roots may need discectomy or laminectomy surgery.
Patients who have suspected or frank instability of the spine may need to undergo fusion surgery as an adjunct procedure in which screws and rods are inserted to stabilize the spine. These patients may also need some bone graft which may be taken from the patient himself or cadaveric bone graft or artificial bone graft with or without use of adjunct bone morphogenic protein. These patients are in the hospital for 2 to 5 days and are allowed ambulation immediately after surgery depending on their recovery from anesthesia.
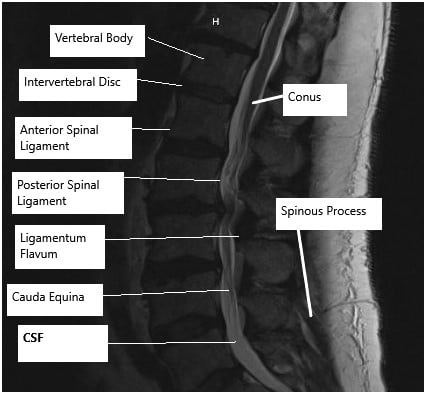
MRI of the lumbar spine
LUMBAR DISCECTOMY
This surgery is usually done for patients who have nerve root compression due to disc herniation, extrusion or sequestration. In this surgery, the aim is to remove the disc fragment, which is causing pressure on the nerve root. This surgery is done for the back and a limited amount of bone is removed as far as we get access to the disc. The disc fragment, which is causing pressure on the nerve root is removed and the nerve root is checked to be free of any pressure. This surgery does not involve removal of enough bone to need stabilization surgery or fusion surgery. The patients after the surgery usually recover well within the next 3 to 6 weeks.
DECOMPRESSION OR FORAMINOTOMY
This surgery is usually done for the patients who have nerve root compression at the level of the foramina. This surgery is done from the back and usually involves removal of a small amount of bone, which is not enough to cause instability. This surgery is not associated with fusion surgery. The patients recover well after the surgery in over the next 4 to 8 weeks.
LAMINECTOMY
Laminectomy involves removal of the bone from the back of the nerve roots. This was performed at one or multiple levels depending on the level of stenosis. This surgery is done from the back. This surgery allows decompression of the nerve roots within the spinal canal. It is consistent and good results and the patients recover well over the span of 6 to 12 weeks.
SPINE FUSION
Spine fusion in the lumbar area is usually performed for instability of the spine or spondylolisthesis. This involves fixation of the vertebrae with screws and rods. It can be done at multiple levels depending on the need. This surgery is usually associated with cleaning of disc space and replacing it with cage and bone graft to make the adjacent vertebrae fuse. This surgery is most commonly performed from the back though it can be performed from the front as well as from the side too. The patients who undergo this surgery usually must be admitted in the hospital for 3 to 5 days and the recovery is gradual for a period of 8 to 12 weeks.

Torque driver with counter torque used in minimally invasive posterior spinal fusion

Rod measuring caliper used in minimally invasive posterior spinal fusion

Castle nut driver used in minimally invasive posterior spinal fusion
The images above show the instruments used in minimally invasive posterior spinal fusion. The minimally invasive technique utilizes the percutaneous incisions to minimize soft tissue trauma. The technique may result in early rehabilitation and reduced post-operative pain.
PREOPERATIVE WORKUP
The patients are usually seen by the physician and appropriate preoperative investigations including advanced imaging, blood work and ECG and chest x-rays as needed are done. The patients may also need clearance from their primary care physician and anesthesiologist before the surgery. The patients are instructed to come to the hospital two hours in advance with no jewelry. The patients are taken to the preoperative area where they are seen by the anesthesiologist and appropriate procedure performed before the patient is taken to the operating room. In the operating room the patient usually is given general anesthesia and intubated before being positioned for the surgery.
POSTOPERATIVE CARE AND RECOVERY
The patients who undergo lumbar spine surgery are usually extubated after the surgery and some patients who undergo surgeries like discectomy and laminectomy can be discharged home on the same day if they meet the criteria to discharge. Most of the time lumbar spine surgery patients are admitted to the hospital for one to five days depending on the surgery and recovery. Patients can mobilize in and out of bed with or without a back support depending on the surgery and recovery from anesthesia. Immediately after the surgery, the patients are encouraged to do their activities of daily living from the first postop day. The patients are provided with medications in the hospital as well as for home to take care of pain and muscle spasms that can develop after the surgery. Incisions need to be kept clean and dry. The patients are instructed to avoid bath and hot tubs, swimming, heavy lifting, driving and smoking. The patients can take shower and remove the dressings after 72 hours from surgery and replace it with dry dressing. The patients are advised to eat healthy and nutritious diet with lot of fibers. The patients are also instructed to use over-the-counter laxatives for constipation that may develop due to pain medications.
RISKS AND COMPLICATIONS
As for all surgeries there are certain but rare risks for anesthesia including cardiac arrest, stroke, paralysis, and rarely death.
Risks of Lumbar spine surgery may include though not limited to:
- Hematoma or hemorrhage
- Damage to the major vessels which may result in excessive bleeding, even death
- Blindness
- Damage to the dura, resulting in a cerebrospinal fluid leak
- Failure, loosening or pull out of the cage, graft, rod or screws
- Wound infection
- Failure of fusion to happen
- Damage to the nerve root(s) resulting in new onset or deterioration of preexisting pain, weakness, paralysis, loss of sensation, loss of bowel or bladder function, impaired sexual function, etc., which may or may not recover.
- A few of these conditions may warrant repeat surgery
Certain patient population is at a higher risk for complication which include but are not limited to:
- Smoking
- Seizures
- Obstructive sleep apnea
- Obesity
- High blood pressure
- Diabetes
- Other medical conditions involving your heart, lungs or kidneys
- Medications, such as aspirin, that can increase bleeding
- History of heavy alcohol use
- Drug allergies
- History of adverse reactions to anesthesia
WHEN TO VISIT AN EMERGENCY ROOM AFTER A SURGERY:
- Suspected cardiac problem: severe chest pain or pressure, shortness of breath, tightness in chest, pain in left arm, jaw pain, dizziness or fainting, unexplained weakness or fatigue, rapid or irregular pulse, sweating, cool, clammy skin, and/or paleness
- Suspected Stroke: trouble speaking, changes in vision, confusion or other change in mental status
- Suspected venous thrombosis: swelling of the legs, ankles, or feet, discomfort, heaviness, pain, aching, throbbing, itching, or warmth in the legs, sudden shortness of breath, chest pain, coughing up blood, rapid or irregular heart rate
- Suspected Sepsis: high grade fever, with shivers associated with fatigue, dizziness, racing heart, pale or discolored skin, sleepy, difficult to rouse, confused, short of breath
- Heavy bleeding from the surgical site
- Severe allergic reaction with trouble breathing, swelling, hives
WHEN TO CONTACT A DOCTOR’S OFFICE AFTER SURGERY:
- temperature more than 101 degrees Fahrenheit
- increased pain or tenderness near the incision
- poor pain relief
- signs of infection: increased swelling, redness, increased drainage, increased warmth, pus, foul smell, bleeding at the incision, incision coming apart
- increased numbness, numbness in genital area
- inability to feel or move fingers or toes
- pale blue, white or abnormally cold fingers or toes
- nausea (upset stomach) or vomiting (throwing up) that won’t stop
- increased tiredness
- a generally worse feeling than you had when you left the hospital
- problems urinating, severe constipation or severe diarrhea
- a concern about any other symptoms that seem unusual

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
