Case Study: Knee Arthroscopy: Medial and Lateral
Meniscectomy and Chondroplasty performed
to 56 year old female patient
An essential diagnostic and treatment aid for the management of knee disorders is knee arthroscopy. Meniscectomy, loose body removal, chondroplasty, microfracture, irrigation and debridement, and tendon reconstruction are examples of indications.
In this set of articles, we provide an in-depth analysis of Patellofemoral Chondroplasty and Partial medial Meniscectomy.
Chondroplasty refers to the smoothing of degenerative cartilage and trimming of unstable cartilage flaps to stabilize and treat chondral lesions. Partial meniscectomy involves trimming unstable flaps of a torn meniscus to establish a stable remnant meniscus.
Patient is a 56 year-old female and has been experiencing right knee pain for almost a week. She is currently working but has to stop because of the knee pain. Considering acute pain with no relief in the last 2 weeks and she is unable to carry out activities of daily living we agreed to do a stat MRI of the knee.
Aside from this, I prescribed Relafen for anti-inflammatory. X-ray and MRI results were presented in the office. X Ray results showed moderate osteoarthritic degenerative changes and slight.
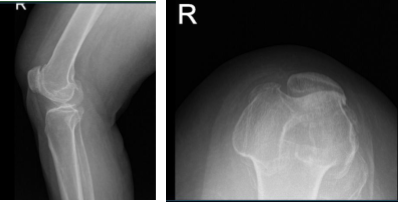
MRI of right knee
MRI result impression as follows: Bone marrow edema at the anterior peripheral aspect of the medial tibial plateau with slight flattening and irregularity of the articular surface there is a low-grade healing subchondral impaction or stress fracture.
Complex tear of the posterior horn medial meniscus including a displaced meniscal flap abutting the posterior root and measures 1 cm in length. Severe patellofemoral arthrosis. Moderate femorotibial arthrosis. Moderate joint effusion.
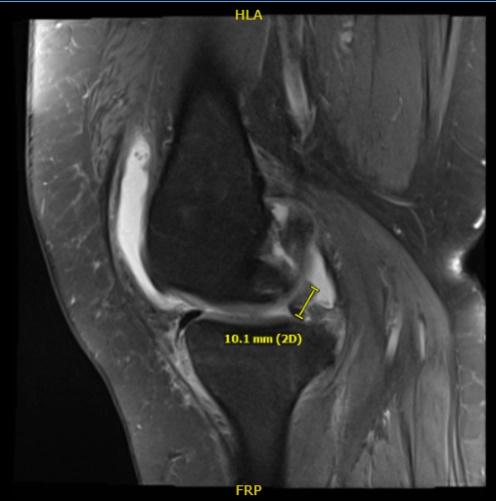
MRI of right knee
She was diagnosed to have a medial meniscus tear and subchondral stress fracture of the medial tibial plateau. Clinically, she had pes anserine bursitis also apart from the other symptoms. We managed her conservatively, but the symptoms worsened.
We discussed treatment options and opted for surgical management. We discussed the risks and benefits including Infection, bleeding, nonunion, nonhealing, need for repeat surgery, need for joint replacement, needing knee rehabilitation, Injury to adjacent nerves and vessels, systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was Induced. The right lower extremity was prepped and draped aseptically in usual fashion. A time-out was called. Preoperative antibiotic was given.
A lateral entry portal was made and an arthroscope entered. Examination of the knee showed a large osteochondral grade 3 to grade 4 lesion of the medial femoral condyle. A medical entry portal was made. Complex tear of the posterior horn of the medial meniscal was found.
Debridement of the medial meniscus tear was done using biter as well as shaver. Once the medial meniscus tear was adequately balanced, the scope was entered into the intercondylar notch. The ACL was found to be intact. There was degeneration of the ACL.
Lateral compartment was examined and found to have medial fraying and tearing of the lateral Shaver was used to clean up the meniscus. There was a small grade 1 to grade 2 osteochondral lesion of the left lateral condyle, which was cleaned using a shaver.
The scope was entered in the patellofemoral joint where grade 3 to grade 4 changes were found in the Inferior medial and lateral facet of the patella as well as trochlea. Debridement was done. The knee was again examined from the medial entry portal and findings confirmed.
Now, the attention was moved to the fixation of the stress fracture of the medial tibial plateau. Cannula was entered from the sub chondroplasty set medially under C-arm control about a centimeter below the joint surface. It was inserted in an anterolateral direction.
The cannula was checked In AP and lateral view and found to be in adequate position. The sub chondroplasty calcium phosphate cement was inserted using 1 cc syringes. Five syringes were used. The cement could be seen filling up the medial tibial plateau region superiorly, superior to the cannula.
Ten minutes were given for the cement to set. The cannula was removed. Final picture was taken and saved. One cc of cortisone with 10 cc of lidocaine was injected. Half percent lidocaine was injected into the pes anserine bursa. One cc of 40 mg of Depo-Medrol with 90 mg of 0.5% lidocaine was Injected Into the knee Joint.
The wounds were closed using #3-0 nylon. The wounds were dressed using Xeroform, 4×4, Webril and Ace wrap. The patient was moved to recovery after extubating in stable.
Patient returned after one week post-operative. General Appearance: swelling and tenderness and wound clean and dry, no warmth, appropriate range of motion, and neurovascular intact.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches during today’s visit. We will continue with ice and elevation of the knee to decrease swelling and pain.
Patients regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

