Case Study: Knee Arthroscopy: Repair of the Lateral Meniscus
Chondroplasty of Patella and Lateral Femoral Condyle
in a 30-year-old Man
Knee injuries involve trauma to one or more tissues like ligaments, tendons, cartilage, bones and muscles. These injuries may happen due to a fall, forceful twisting of the knee or any accident. Common knee injuries include fractures, dislocations, tears and sprains.
The patient came to the office with a complaint about his right knee pain. He stated that he injured his knee while getting out of the swimming pool and felt a “snap” in his right knee. He stated that the severity of pain is severe.
Timing of pain is constant and it disturbs while he sleeps. There is also swelling, weakness and limping. Patient is ambulatory with a walker. He was having a hard time doing his physical activities. He said rest helps him with the symptoms. He had knee surgery in 2013-2014.
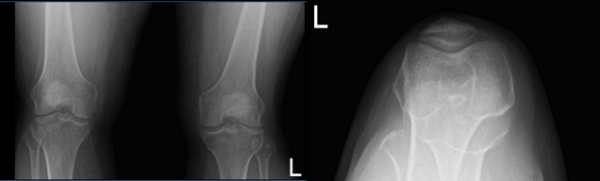
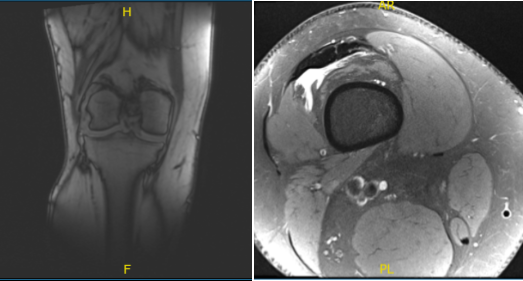
An MRI and X-ray were performed, which shows lateral meniscus tear. We discussed treatment options and the patient opted for surgical management. We discussed the risks and benefits and complications of the surgery. We discussed possible meniscal repair versus meniscectomy. The patient understood and signed an informed consent.
Arthroscopic surgery was performed. Lateral anterior portal was made for arthroscopic viewing. The scope was entered and the camera was entered. The camera showed a tear of the posterior horn and brought the posterior body of the lateral meniscus around the popliteal hiatus at its periphery.
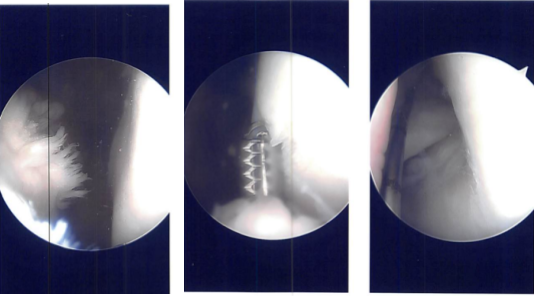
The tear was repairable and I decided to repair it. There was a grade 2 to grade 3 chondral lesion over the patella as well as lateral condyle of the femur. Chondroplasty was performed. The meniscal rasp was used to prepare the capsular as well as the meniscal attachment.
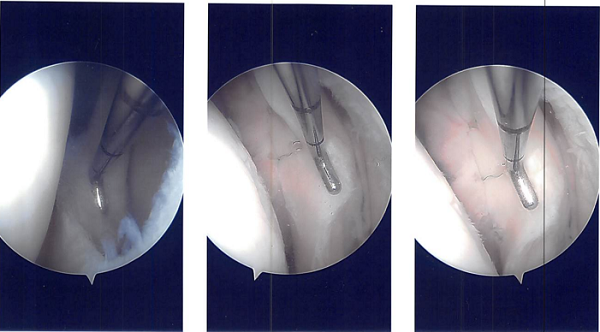
A plane was made between the popliteus and the gastrocnemius with the vessels behind. Sims speculum was used to retract the vessels posteriorly. Another scope was reintroduced on the lateral border and all-inside repair was done using FasT-Fix with a Nephew curved all-inside implant and sutures.
Three of them were put in the body posterior and medial to the popliteus muscle and one was put lateral to the popliteus muscle. The reduction and repair were found to be adequate. The tourniquet was released and found to have a good blood clot inside.
The Incision was closed. Marcaine 1% 10-cc were put into the joint. Dressing was performed using 4x4s ABD, Webril and Ace wrap. Bledsoe knee brace was put with locked in extension. The patient was moved to the postoperative care unit after extubating in a stable condition.
After a week of postoperative surgery, he had been using a knee brace (ROM) and denied fever and chills. A month after, the incisions were healed well, without evidence of drainage, erythema or warmth. He was advised to do physical therapy and take some anti-inflammatory drugs until he had a full relief.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
