Case Study: Knee Arthroscopy: Medial Meniscectomy and
Medial Femoral Chondroplasty in a 38 year-old patient
The surgical treatment known as knee arthroscopy is less invasive. Knee arthroscopy is used by medical professionals to identify and treat a variety of knee problems. A very long, thin instrument with a camera is then inserted by your healthcare professional after making a tiny incision. Your healthcare practitioner can diagnose your damage thanks to the camera’s photographs of the interior of your knee.
The most frequent cause of knee issues is injuries. A direct hit to the knee may result in sudden (acute) damage. Alternatively, they might be brought on by unnatural twisting, knee bending, or landing on the knee.
Within minutes after the accident, there may be considerable pain, bruising, or swelling. During the injury, blood vessels or nerves might be injured or squeezed. The lower leg or knee may feel weak, numb, or chilly. It could tingle or seem blue or pale.
A 38 year-old patient visited our office with complaints regarding right knee pain due to a motor vehicle accident. She had no pain in her neck, back or right knee prior to the accident. She has tried PT with no relief. She smokes but plans to quit.
For aggravating factors, patients report standing, walking, lifting, twisting, weight bearing, exercise, upstairs, and downstairs.
For associated symptoms, she reports weakness, tingling, and pain with motion but reports no numbness, no swelling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
For location, she reports right. For quality, she reports aching, burning, throbbing, frequent, and no change. For severity, she reports moderate. For timing, she reports chronic. For alleviating factors, she reports rest and lying down. For previous surgery, she reports none.
She presented an MRI result that showed free edge truncation and radial tearing involving the medial meniscal body in which its remnant is partly extruded outside the medial tibiofemoral joint compartment.
Radial tearing extends into the anterior horn-body junction anteromedially. Strain of the medial collateral ligament at its femoral attachment site is present. Some edemas are superficial to the medial collateral ligament toward its anteromedial margin.
Edema in the prepatellar and pretibial subcutaneous tissues. Synovial fluid anteriorly at the tibiofemoral articulation and at the patellofemoral articular surface extending slightly laterally more than medially.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all of the discomfort. Also, I explained there is no guarantee all the function and strength will return. The patient also understands the risks of re-tear or failure to heal. The patient understands implants may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. Ample time was given for questions, of which many were addressed. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was Induced. Preoperative antibiotics were given. A tourniquet was applied over the lower thigh.
The right lower extremity was prepped and draped aseptically in the usual fashion and put in the knee holder. A lateral entry portal was made. Arthroscope was entered. Medial entry portal was made with a use of spinal needle.
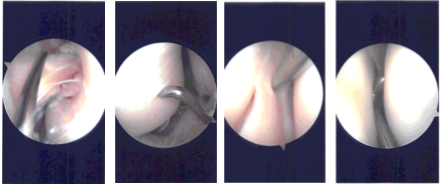
Examination of the medial compartment showed frayed tearing of the anterior horn of the medial meniscus. Shaver was used to clean up the meniscus. Balanced margins were achieved. There was no tear of the body of the posterior horn. The root was intact.
Medial femoral condyle showed grade 1 to grade 2 osteochondral lesion, which was cleaned up with a shaver. Examination of the intercondylar notch showed intact ACL. Examination of the lateral compartment showed intact lateral meniscus as well as intact cartilage of the lateral tibiofemoral compartment.
Examination of the patellofemoral compartment showed no lesion of the patellofemoral cartilage. Patellar tracking was proper. Examination of medial and lateral gutters showed no loose body. The scope was inserted from the medial condyle and the findings were reconfirmed. Final pictures were taken and saved.
The knee was thoroughly irrigated and drained. Closure was done using # 3-0 nylon. Then 9 cc of Marcaine 0.5% mixed with 40 mg of Depo-Medrol was injected into the knee. Dressing was done using Xeroform, 4 x 4, ABD, Webril, and Ace wrap. The tourniquet was released and the patient was extubated and moved to recovery in a stable condition.
The patient had a twisting injury and injured the knee. She was complaining of worsening right knee pain. MRI was performed again which showed tear of lateral meniscus.
The patient was taken to the operating room area where she was placed on a well-padded operating room table. General anesthesia was induced. Tourniquet was applied. Preoperative antibiotic was given. The right lower extremity was prepped and draped aseptically in the usual sterile fashion.
A lateral entry portal was made. Arthroscope was inserted and a medial entry portal was made for entry of the instruments. Examination showed a lateral margin fraying of the medial meniscus which was debrided with the use of shaver and Coblation wand.
There was no arthritis of the medial tibiofemoral compartment. Examination of the intercondylar region showed intact ACL. Examination of the lateral tibiofemoral compartment showed tear in the anterior horn of the lateral meniscus, which was debrided with the use of shaver and Coblation wand.
There were no arthritic changes. Examination of the patellofemoral compartment showed grade 1 to grade 2 arthritic changes in the patella, which was cleaned with the Coblation wand. Superior plica was found to be inflamed and was excised with the use of Coblation wand. and shaver.
The knee was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon. Then 9 cc of Naropin mixed with 1 mg of Depo-Medrol was injected into the knee. Dressing was done with the use of Xeroform, 4 x 8s, ABD, Webril, and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
We have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient did well after the surgery and continued physical therapy. The patient checked in for a follow up visit after a month and saw significant improvement in her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
