Case Study: Robotic Left Hip Total Replacement
for Arthritis secondary to Avascular Necrosis of the Hip
The patient was a 59-year-old male presenting as a new patient for consultation regarding his left hip pain. The hip pain started insidiously 2 years ago and progressed gradually. He was previously diagnosed with avascular necrosis of the left hip by an outside physician.
He was working as a security officer at an airport but was currently on leave secondary to hip pain. He denied any history of fall or trauma or long term steroid intake. He was a nonsmoker and consumed alcohol socially.
He reported the pain as a dull ache located in the left groin radiating to the left knee. The pain was moderate to severe in intensity (7/10). The patient reported increased severity of pain on activities such as walking, bending, sitting, squatting and going up or down the stairs.
The patient used a cane for ambulation and received two hip cortisone injections with minimal relief. He also had a trial of physical therapy with no relief. The patient was distressed having not been able to do his daily activities. He had given up riding his bicycle, a hobby he enjoyed for the past many years.
His past medical history included coronary heart disease, liver dysfunction, benign prostate hypertrophy, and dyslipidemia. All his medical conditions were well controlled with medications. His past surgical history included a right shoulder arthroscopic surgery and laparoscopic cholecystectomy done 6 years ago.
On physical examination, his gait was antalgic with a decreased stance phase on the left side. Both the shoulders, iliac spines, patella, and medial malleolus were at the same level. There was no evidence of any exaggerated lumbar lordosis and scoliosis.
There were no enlarged inguinal lymph nodes or any fullness in the groin region. The skin overlying the left hip was normal with no scar, sinus or redness. There was tenderness over the left hip anterior joint line. The range of motion was restricted in the abduction and internal rotation.
The bulk and power of both the extremities were intact. There was no deficit of light touch in all sensory dermatomes of the lower extremities. Examination of the right hip, both knees and ankles were normal. Bilateral dorsalis pedis and posterior tibial pulses were palpable and good volume.
Imaging revealed severe osteoarthritis of the left hip and an MRI suggested avascular necrosis changes in the left hip. In view of lifestyle limiting hip pain and patients’ comorbidities, a robotic total hip replacement was advised to the patient. Risks, benefits, and alternatives were discussed at length with the patient. He agreed with the plan. A preoperative CT scan was also obtained.
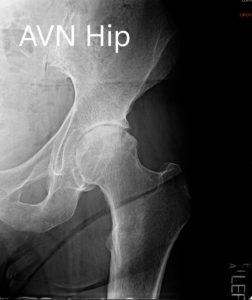
Preoperative X-ray showing the AP and the lateral views of the left hip.
PREOPERATIVE DIAGNOSIS(ES): Left hip arthritis secondary to avascular necrosis.
OPERATION: Robotic left total hip arthroplasty.
IMPLANTS USED: Size 58-cup and liner, screw size 6.5 x 30 mm with a 127-degree size 11 stem with a 36 mm head.
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining the informed consent, signing on the correct surgical site. The risks, benefits, and alternatives were extensively discussed with the patient as well as with her husband prior to the procedure. The patient was then anesthetized by the anesthesiologist and the left hip was then draped and prepped in the usual sterile manner.
Robotic arrays were used by placing the external fixator over the iliac crest. The incision was made over the hip and the skin and subcutaneous tissues were incised. The fascia was then divided. The posterior soft tissue structures were then taken down and the hip was then dislocated. The microdissection was made over the correct level.
The head was removed. The acetabular rim was then exposed. The remainder of the labrum was then debrided. The acetabulum was then sequentially reamed after making robotic calibration and the cup was then placed into position in the correct abduction and anteversion. A screw was placed for additional fixation, the poly was then placed over the shell. Thorough lavage was given. Attention was then turned towards the femur. The femur was then sequentially broached.
The final broach was placed into position, and the trunnion and head were then placed and hip was then reduced and trialed through a full range of motion. Hip was found to be stable in all physiological range of motion. A preoperative CT scan was then compared to the final measurements and the measurements on the robotic system were found to be accurate.
The hip was then dislocated. Trial components were then removed. Final components were then placed into position and the hip was then reduced. The robotic system measurements were then again measured and were found to be correct. Screws for the markers were then removed from the femoral as well as the acetabular part of the hip.
Thorough lavage was given. Posterior soft tissue structures were then packed with intertrochanteric through transverse tunnels. The fascia was closed with Ethibond. Cutaneous tissues were closed with O Vicryl. Subcuticular tissues were closed with 2-0 Vicryl. The skin was closed using Monocryl. Sterile dressing was then applied over the wound, and the patient was returned to the postoperative care in stable condition.

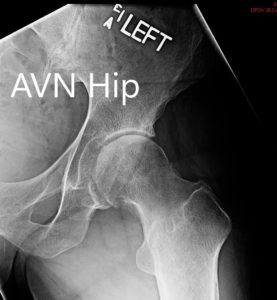
Postoperative X-ray of the pelvis with both hip joints in the AP view.
The patient’s pain was well managed with medications. An abduction pillow was given to the patient and hip precautions were explained. Thrombotic-Embolic-Deterrent (TED) stockings and aspirin were prescribed to prevent deep vein thrombosis. Weight-bearing was allowed as tolerated with support. Physical therapy was started to increase range of motion and strengthen muscles.
The patient’s recovery was excellent in three months. He was walking with no pain and with no support. He had successfully concluded his physical therapy. He was advised to stop aspirin and wean off hip precautions gradually. He was back riding his bicycle and happily back to his job. The patient expressed great satisfaction at the outcome of the procedure.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
