Case Study: Knee Arthroscopy: Medial and Lateral
Meniscectomy, Cyclops Excision and Chondroplasty
performed to 61-year-old male patient
Knee arthroscopy is an important diagnostic and treatment tool for the control of knee disorders. Indications include meniscectomy, loose body removal, chondroplasty, microfracture, irrigation and debridement, and tendon repair.
We examine Patellofemoral Chondroplasty and Partial Medial Meniscectomy in depth in this series of papers.
Patient is in our office with complaints of left knee pain for over 6 months now. The patient remembers no injury. The pain is severe in intensity. Patient describes the pain as throbbing. The pain is constant, and does disturb sleeping.
The pain is associated with swelling, limping. The pain is not associated with bruising, tingling, numbness, radiating pain, weakness, bowel or bladder abnormality, gait problem, giving way, hand function difficulty. The problem has been getting worse since it started.
Walking, standing, bending, squatting, kneeling, and stairs make the symptoms worse. Heat, applying Bengay, knee wrap makes the symptoms better. The patient has undergone surgery for meniscus repair approximately 10 years ago.
He presented his X-ray and discussed the results. There are no degenerative changes found. However, fracture of enthesophyte arising from the proximal patellar tendon.

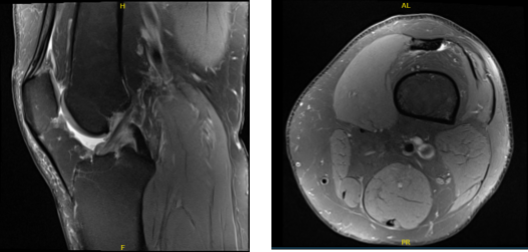
MRI presented after a week, and found medial meniscal tear with dominant radial component posterior horn with peripheral extrusion.
Osteoarthrosis with moderate to high-grade cartilage loss peripheral aspect of the medial compartment and a focal 3.5 x 14 mm moderate to high-grade cartilage defect along the lateral trochlear cartilage. Indeterminate lesion distal femur likely a probable enchondroma and small joint effusion were found.
Upon examination of the left knee, the patient is tender to palpation along the lateral joint line, and has an effusion. Patient also has PF crepitus and tenderness on palpation along the medial and lateral PF joint line. Patellar grinding test is positive.
The patient has discomfort with McMurray’s maneuvers, and the knee is stable. They lack full flexion secondary to the effusion, but have full extension. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present.
We discussed risks and benefits of surgical treatment including infection, bleeding, failure to heal, need for repeat surgery, injury to adjacent nerves and vessels, blood clots, neurological, pulmonary, cardiac complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. Left lower extremity was prepped and draped aseptically on the tourniquet. IV antibiotic was given before inflation of the tourniquet.
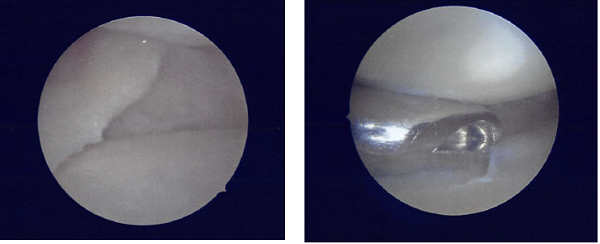
A lateral entry portal was made and an arthroscope was inserted. Examination of the knee showed a tear of the medial meniscus posterior horn.
A medial working portal was made using a spinal needle followed by an incision. Further examination of the knee showed a cyclops lesion of the ACL as well as medial frayed margins of the lateral meniscus.
There was grade 1 to· grade 2 osteoarthritic changes in the medial femoral condyle as well as grade 3 to grade 4 osteoarthritic changes in the trochlea. The tear of the medial meniscus was compact and was not repairable.
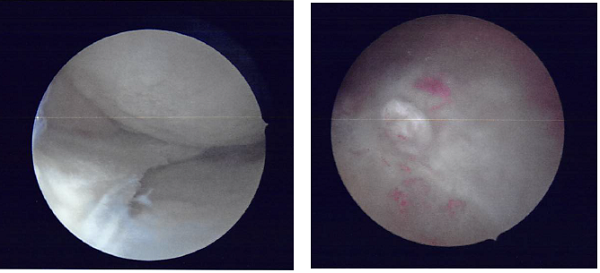
I performed a partial meniscectomy using a shaver as well as straight and upbitters. A balanced margin was reached. Following that the shaver was moved to the intercondylar notch where the cyclops excision was performed using the shaver.

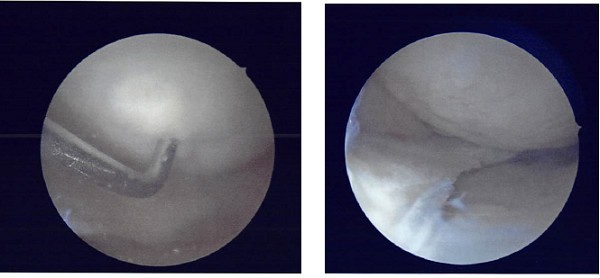
The shaver and the arthroscope was moved to the lateral compartment where partial meniscectomy of the medial frayed margins of the lateral meniscus was performed using the shaver. Chondroplasty of the medial tibial condyle as well as chondroplasty of the trochlea was performed using the shaver.
Final pictures were taken and saved. The knee was irrigated thoroughly and drained. The arthroscope was removed. The closure was performed using #4-0 Vicryl and #3-0 nylon.
Dressing was performed using 4 x 4, ABO, Webril, and Ace wrap. The patient was extubated and moved to the Recovery in a stable condition.
After a week of seeing the patient, he has been improving with regards to pain and swelling. He is limping and has been using crutches for ambulation.
Denies fever, chills, reinjury. After two weeks post surgery the incisions are healing well, without evidence of drainage, erythema or warmth.
There is a full range of motion without discomfort. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee.
The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.

