Case Study: Distal Biceps Repair in a 52 year-old patient
A distal biceps repair involves your doctor reattaching the torn biceps tendon to the radius, one of the lower arm bones, during surgery. Your surgeon could suggest distal biceps tendon repair surgery if there is a delay in having surgery.
The majority of patients have an abrupt popping or tearing feeling at the front of their elbow along with severe pain throughout their upper forearm and lower arm. It typically occurs after lifting or lowering a large burden. Following this pain, there is swelling and bruising in the forearm and elbow crease.
A 52 year-old patient was in our office with complaints regarding the injury to left elbow when a heavy weight slipped off his left hand. For aggravating factors, patients reported twisting, pushing/pulling, and weightbearing. For location, he reports left. For quality, he reports aching.
For severity, he reports moderate. For associated symptoms, no weakness, no numbness, no tingling, no swelling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
For previous surgery, he reported none. The patient’s MRI result was reviewed and discussed. The results showed biceps tendon rupture and lateral epicondylitis.
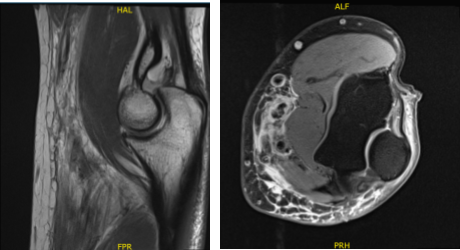
MRI 3T Left Elbow non-contrast
We discussed treatment options and the patient opted for surgical management. We discussed risks and benefits and complications including infection, bleeding, injury to adjacent nerves and vessels, numbness, failure, need for repeat surgery among others.
We discussed this rehabilitation among others. We discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. Right upper extremity was prepped and draped aseptically in a usual fashion. Supraclavicular block was already given. Sterile tourniquet was applied.
An Esmarch was applied and the limb was exsanguinated. A transverse incision of about 4 cm was given, 2 cm distal to the distal elbow crease anteriorly. With sharp and blunt dissection, the subcutaneous tissue was reached.
With finger dissection, the biceps tendon could be seen, which was detached, but was lying in position. The tendon was extracted outside of the incision. The tendon was prepped and whipstitch suture was given with the use of FiberLoop.
The tendon insertion point was also repaired by debridement. Now, the tendon was sized to be at 7 mm. Radial tuberosity was found with the distal palpation and diamond-tip Beath pin was passed bicortically with the use of drill.
A unicortical drilling with 8 mm drill was performed to allow 7 mm bioabsorbable endoscope. The suture of the FiberLoop was loaded onto an EndoButton and was passed bicortically and the button was stripped and tightened.
The suture was passed with tendon and tied on to each other to achieve the second part fixation. The EndoButton was inserted over the tendon and a third point of fixation was achieved well. The wound was thoroughly irrigated and drained. Tunica was released.
There was no active bleeding. Closure was done in layers using #2-0 Vicryl and # 3-0 Monocryl. Dressing was done with the use of Xeroform, 4 x 4, Webril, posterior splint and Ace wrap. The patient was extubated and moved to recovery in a stable condition. He was put in a shoulder sling.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the elbow. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his elbow.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
