Case Study: Implant nail removal performed
to a 87-year old female after experiencing pain
Untreated bone fractures can result in either nonunion or delayed union. In the earlier case, the bone does not heal at all, so it remains broken. As a consequence, swelling, tenderness, and pain will increase over time.
Patient presented today in the office was an 87-year-old female, with complaints of left femur and left knee pain. The pain is severe in intensity. The pain is constant. The problem has been getting worse since it started. Walking and standing make the symptoms worse.
Rest is the only option to make the symptoms better. The patient has undergone trochanteric fixation surgery for her left femur on August 24, 2014. She has been using a walker for ambulation since then. She has had viscosupplementation in the past with no benefit. She feels the pain is more in the front of her knee.
Upon examination of the left knee, the patient is tender to palpation along the medial and lateral facets of the patella as well as along the medial knee joint line and distal femur.
They have crepitus of the patellofemoral joint with range of motion and discomfort with patella grind testing. The patient has discomfort with McMurray’s maneuvers, and the knee is stable.
They have limited range of motion. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability and strength.
Xray were presented and reviewed, the patient’s femur was healed intertrochanteric fracture but there are mild osteoarthritic degenerative changes found on her knee. We discussed the possibility of etiology of knee pain and treatment options.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 3cc of 1% lidocaine, 3cc of 0.5% Marcaine and 80 mg of depo-Medrol were injected into the left knee.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
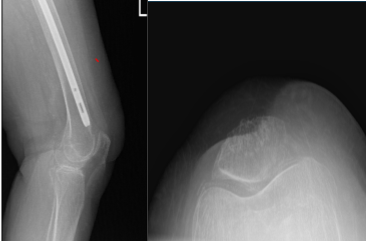
Left Knee X-ray Complete with Patella
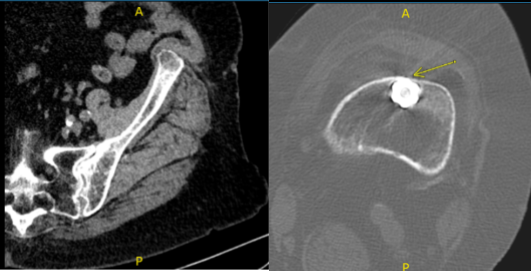
After 6 weeks from the first visit, the patient returned with a CT scan result, it was reviewed and ruled out our impingement, and there were mild degenerative changes of the left hip and presents atherosclerotic disease.
Also found that the distal tip of the femur impinging on the anterior cortex of the femur with erosion. We discussed treatment options including operative and nonoperative treatment.
The patient operated for operative management. We discussed the risks, benefits and complications of operative management including infection, bleeding, non resolution of the pain, refracture and need for repeat surgery among others. The patient understood the risks and complications well and signed an Informed consent.
The patient was taken to the operating room where she was placed on a well-padded operating table. General anesthesia was induced. The pump was put under the left hip. A C-arm was brought in to see that the table end position allowed adequate imaging.
The left lower extremity was prepped and draped aseptically in a usual fashion. A time-out was called. Preoperative antibiotic was given. Incision was driven over the tip of the trochanter. The incision had to be extended to allow adequate exposure. The trochanter was reached and the needle tip could be seen.
The screwdriver was used to remove the end cap. After that, the outer nail sleeve was inserted and a flexible driver was inserted to loosen the setscrew.
Then, a lateral incision was driven over the previous incision and the lateral cortex of the femur was fished. The hip screws could be felt and the screwdriver for the hip screw was inserted and adequately tightened. It was checked with the C-arm.
Slot hammer was used to remove the hip blade. Once the hip blade was removed, the slot hammer was used proximally to remove the nail also. Once the nail was removed, deep culture was sent.
The wound was washed copiously. Closure was done in layers using Vlcryl #0, Vlcryl #2-0 and Monocryl. Dressing was performed. The patient was moved to the postoperative care unit in a stable condition.
Patient returned to the office for post operative follow up. She presented the result of her CT scan, 4 weeks after the operation and there are mild osteoarthritic degenerative changes.
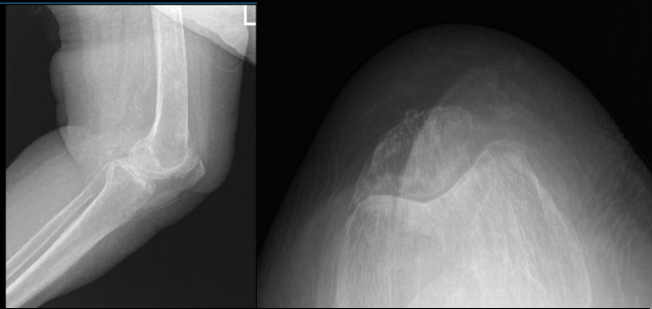
Left Knee X-ray AP and Lateral with Oblique 3 views
Patient condition gets better. She is doing well. She has stopped using a walker for a short distance and is without one today. denies fever, chills.
Gait training and Physical therapy were introduced to the patient, agreed to proceed and continued follow up were advised. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
