Case Study: Right Knee Arthroscopy: Medial Meniscectomy
Lateral Meniscectomy, and Chondroplasty
in a 61 year old female
A cartilage component called meniscus, aids in the appropriate function of your knee. Meniscal tears, a frequent knee ailment, are commonly treated by a meniscectomy.
The purpose of the procedure is to eliminate meniscus pieces that protrude into the joint. Your knee may lock as a result of these pieces obstructing joint mobility.
Your meniscus tear may heal naturally or need to be surgically repaired if it is on the outside third of the meniscus. This is due to the fact that blood cells in this region, which are abundant, can renew meniscus tissue or aid in its recovery following surgical repair.
Nevertheless, if the rupture is in the innermost there is no blood flow—it cannot be mended and might have to be surgically trimmed or eliminated.
A 61-year-old patient was in our office, with complaints of right knee and leg for months now. The pain is severe in intensity. She described the pain as sharp, dull, stabbing, throbbing, aching which are also associated with swelling, bruising, tingling, radiating pain, weakness, giving way and limping.
However, the pain is not associated with numbness, bowel or bladder abnormality, gait problem, hand function difficulty but walking, standing, exercise, bending, squatting, kneeling, stairs, sitting make the symptoms worse. Using ice makes the symptoms better. The patient has undergone previous surgeries.
She does not smoke. Her knee MRI right shows radial tear through the posterior horn of the medial meniscus. She has tried bracing, ice, elevation, and anti-inflammatory medications but has had no relief. Her calf pain has relieved and is no longer there. Her main concern is her knee pain. She is using a cane to ambulate.
Upon examination of the right knee, the patient is tender to palpation along the medial joint line and has an effusion. She is also tender proximal leg medial to tibia and over the tibial attachment of MCL. The patient has discomfort with McMurray’s maneuvers, and the knee is stable.
They lack full flexion secondary to the effusion but have full extension. They have 5/5 strength and are neurovascularly intact distally. There are no erythema, warmth or skin lesions present.
On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability, and strength.
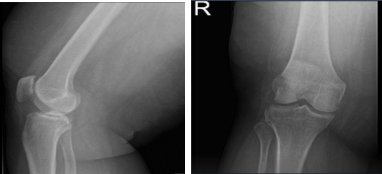
Right Knee X-ray AP Lateral and Oblique
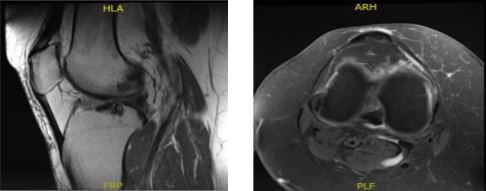
MRI-3T Right Knee Non-contrast
MRI results were presented and shown that there is a radial tear through the posterior horn of the medial meniscus. Tricompartmental cartilage loss, worst in the medial compartment where there is a focal full-thickness chondral defect. There is moderate partial-thickness patellar cartilage loss. Small joint effusion and Baker’s cyst.
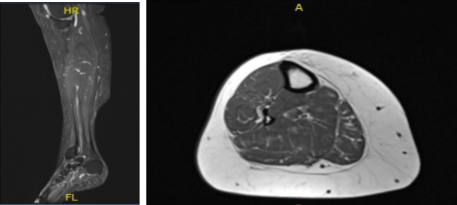
MRI- Right Calf Non-contrast
The patient is here for a follow up with an MRI of the right calf to review. Results showed no evidence of tibial stress fracture or stress reaction. Calf musculature is normal.
Degenerative changes within the knee as well as a small popliteal cyst are better appreciated on the recent knee MRI. Limited evaluation of the ankle demonstrates chronic plantar fasciitis and a partial tear at the origin of the central cord.
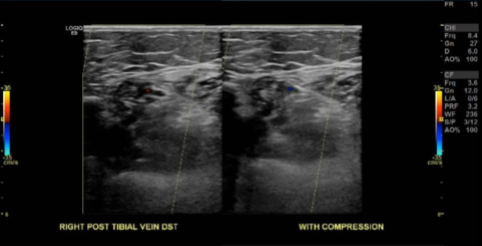
Doppler Venous Right Lower Extremity
The results showed no sonographic evidence for RIGHT lower extremity deep venous thrombosis.
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections, and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to anesthesia, infection, damage to nerves and blood vessels, blood loss, blood clots, and even death were discussed at length.
The patient also understands there is a long rehabilitative process that typically follows the surgical procedure. We talked about the possibility of not being able to alleviate all the discomfort, understands the risks of re-tear or failure to heal, and understands implants may be utilized during this surgery. Despite that, the patient still proceeded with surgery.
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was induced. A tourniquet was applied over the right lower extremity.
The tourniquet was inflated, and the left leg was placed in a well leg knee holder. The knee was prepped and draped aseptically. Preoperative antibiotic was given. A lateral entry portal was made, and an arthroscope was introduced.
The patellofemoral compartment showed osteoarthritic changes. The medial compartment shows osteoarthritic changes as well as complex medial meniscus tear of the posterior horn and the body. The tear was resected using a straight biter or biter and shaver to stable margins.
A thin layer of the posterior meniscal tissue was left in the posterior body. The left femoral condyle chondroplasty was performed using a shaver. Now, the scope was moved to the intercondylar area, where ACL was seen. It was intact but frayed. ACL debridement was performed.
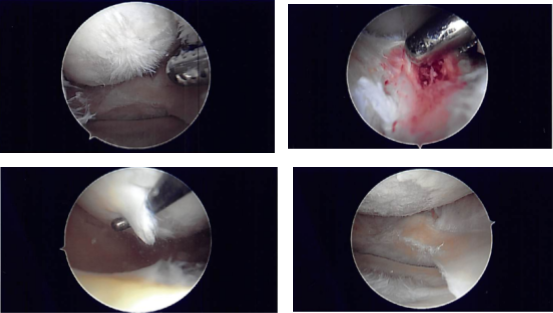
Intraoperative Arthroscopy Images
The scope was moved to the lateral femoral compartment, tibial femoral compartment where there was fraying of the med ial margins of the lateral meniscus as well as tear of the undersurface of the posterior horn of the lateral meniscus. The meniscus was debrided using a shaver.
There were osteoarthritic changes in the lateral femoral condyle, which was shaved. The scope was moved to the patellofemoral compartment, where arthritis was found in the undersurface of the patella as well as the trochlea. It was shaved using a shaver.
The new scope was now introduced into the medial compartment and the findings were rechecked and final shaving was performed. The knee was irrigated.
The closure was done with nylon #4-0; 80 mg of Depo-Medrol with 6 cc of 0.5% Marcaine was introduced into the right pes anserine bursa and 80 mg of Depo-Medrol with 6 cc of 0.5% Marcaine was introduced into the right knee joint.
Dressing was performed using 4×4, ABD, Webril, and Ace wrap. Tourniquet was released. The patient was extubated and moved to the recovery unit in a stable condition.
The patient was seen for post operative check up and has decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We will continue with ice and elevation of the knee to decrease swelling and pain as well as utilizing early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wear them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications, and she will also continue aspirin. I will see them back in three weeks time to evaluate their progress.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
