Case Study: ACL, Arthroscopic Assisted Reconstruction
with Autograft in a 33 year-old male
We use arthroscopic surgery, which is less intrusive and hastens patient recovery, to repair the ACL. The torn ligament is restored during an ACL reconstruction with a tissue graft from either a donor (allograft) or your own body (autograft).
The goal of autograft anterior cruciate ligament (ACL) reconstruction surgery is to repair a ruptured knee ligament. It facilitates pain relief, increases mobility, and enhances athletic performance.
The patient is a 33 year-old male seen in the office with left knee pain due to a car accident along with buckling and giving way. He tried nonoperative treatment but did not help. He had no pain or disability in the left knee before that happened.
An MRI presented and reviewed by the doctor, which showed a tear of the ACL and medial meniscus of the left knee. We discussed treatment options and the patient opted for surgical management.
We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, failure of repair and healing, need for future surgery, arthritis, knee stiffness, need for rehabilitation, possible need for total knee replacement in the future amongst others.
We also discussed systemic complications including blood clots, cardiac, pulmonary, neurologic complications including death. The patient understood and signed an informed consent.
The patient was taken to the operating room where he was placed on a well-padded operating room table. General anesthesia was induced. Preoperative antibiotics in the form of 2 g of Ancef was given. Left thigh was left in a thigh high tourniquet and prepped and draped aseptically in the usual fashion.
The patient was put in a knee flexed position with the leg dangling. Time-out was called. Skin markings were done. The limb was exsanguinated with the use of Esmarch and tourniquet was inflated to 325 mmHg. Tourniquet time was 90 minutes.
Lateral entry portal was used following an incision. Arthroscope was entered. Patellofemoral compartment and medial and lateral gutters showed normal anatomy. Pictures were taken.
Examination of the medial tibiofemoral compartment showed grade 3 to grade 4 osteochondral damage of the medial femoral condyle as well as degeneration of the medial meniscus and tearing.
There was grade 1 to grade 2 osteochondral damage of the medial tibial plateau also. There were no loose bodies out of the meniscus. Examination of the intercondylar notch showed degenerated and ruptured ACL.
Examination of the left tibiofemoral compartment showed lateral grade 3 to grade 4 osteochondral damage of the left femoral condyle and tear of the posterior horn of the lateral meniscus and undersurface of the meniscus.
Graft Plan was made to do quad tendon reconstruction of the ACL. Scope was removed and made. The scope was Midline incision was driven through the superior margin of the patella and quadriceps. The skin, subcutaneous tissue, and the paratenon was cut to the line of incision.
A 10-mm blade was used to cut the quadriceps on either side up to the 60 mm mark. The quadriceps tendon was stripped over from the proximal patella with the use of a knife. Fiber Tank was used to tack the distal quadriceps.
Quadriceps cutter was used to elevate the quadriceps in a sequential manner up to the 80 mm and was cut. The graft was taken to the back table and prepared with the use of and was wrapped with vancomycin-soaked gauze.
In the meantime, medial meniscectomy was performed with the use of shavers. Partial lateral meniscectomy was also performed with the use of a shaver. Chondroplasty was performed again with the shaver on the medial femoral condyle and the lateral femoral condyle.
Once this was done, the ACL was debrided. Medial tibial tunnel was made with the footprint just in line with the lateral meniscus in the posterior margin of the anterior horn of the lateral meniscus and the intercondylar notch.
The tibial tunnel was made with the use of Flip Cutter and a 30 mm tunnel was made. Similarly, a femoral tunnel was made with a femoral jig with the use of 9.5 mm FlipCutter and a 30 mm tunnel was again made.
Both tunnels were secured with the use of Fiber Stick. Now, the graft was brought in. The medial portal was decreased in size and the graft was introduced through the femoral tunnel followed by the tibial tunnel with the use of Fiber Stick loops.
Once they were in position and the markings could be seen, 27 mm was passed into the femoral tunnel and 27 mm was passed into the tibial tunnel. The buttons of the adjustable Tightrope were tied on each other on either side.
The incisions were thoroughly irrigated and closed in layers with the use of #0 Vicryl, #2-0 Vicryl, Monocryl for the quadriceps incision, and nylon # 3-0 for arthroscopic incisions.
Dressing was done with the use of Xeroform, 4 x 8s, ABD, Webril, and Ace wrap. Knee immobilizer was applied and locked in extension. The patient was extubated and moved to recovery in a stable condition.
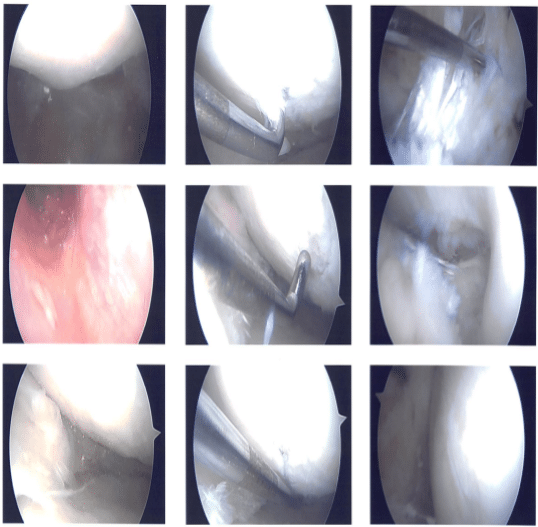
Intraoperative images
After one week from the surgery, the patient is seen in the office for his postoperative visit, no x-rays are needed. His pain control had been good till yesterday when he started having this pain. No injury or accident before the start of pain. We discussed the need for home and outpatient PT.
We also discussed the need to work up if the pain does not subside. After two weeks the patient visits the office for his follow up checkup, no x-rays are needed. His pain control has improved but not started PT yet, he denies fever and chills.
During the visits, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We removed the stitches during the visits. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. Follow up checkup after three weeks.
After a month the patient is here for his postoperative visit, no x-rays are needed. His pain control has improved. He is working with PT and gradually improving, he denies fever and chills.
After the operation, the patient recovered well and kept up with physical therapy. After two months, the patient returned for a follow-up visit and his knee had much improved.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
