Corticosteroids Use & Avascular Necrosis of the Femoral Head
Avascular necrosis (AVN) of the femoral head occurs commonly after long term corticosteroid use. The corticosteroids such as prednisone are prescribed for a number of medical conditions. Long term use is associated with AVN of the femoral head requiring total hip replacement, particularly in younger patients.
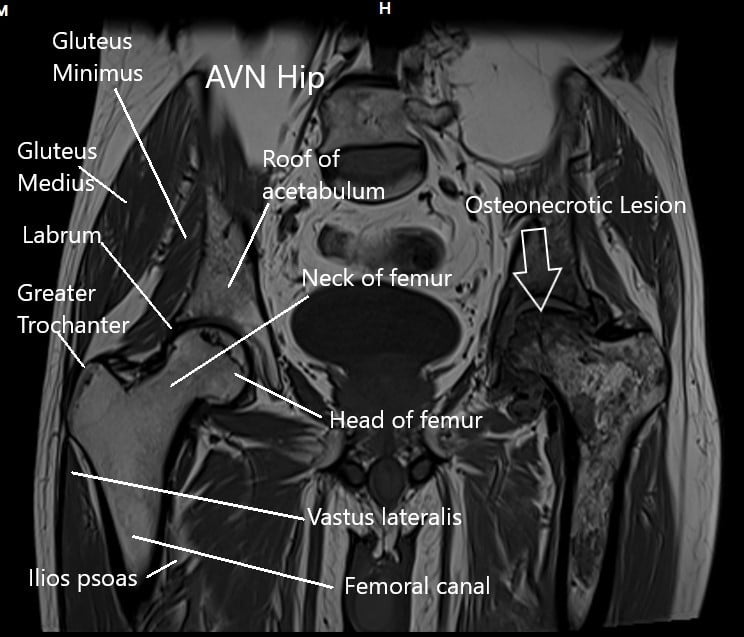
MRI of the hip joints in the coronal section.
Avascular necrosis is due to loss of the blood supply of the head of the femur. This results in subsequent bone death, also known as necrosis. The upper end of the thigh bone (femoral head) forms the ball of the hip joint.
The femoral head has a precarious blood supply. Any disruption may lead to bone death and the collapse of the joint.
Glucocorticoids or corticosteroids are medications used to treat a number of medical conditions. The medication is commonly used in a short duration to decrease inflammation and reduce pain. Long term use of oral corticosteroids is one of the major risk factors for avascular necrosis of the femoral head.
Glucocorticoids are prescribed as a treatment for chronic conditions. Diseases such as nephrotic syndrome, transplant recipients, systemic lupus erythematosus, and a number of skin conditions are managed with corticosteroids. The steroids suppress the immune system and provide relief from autoimmune diseases. Corticosteroids are also illicitly used by athletes and bodybuilders to rapidly build muscle mass.
The majority of the patients with these diseases happen to be young and middle-aged adults. The high incidence of avascular necrosis in these patients is linked with the effects of glucocorticoid therapy.
Corticosteroids reduce the inflammatory cell function in the body. The other effect directly linked with the avascular necrosis is lipogenesis or an increase in lipid/fat content of the blood. The increased lipid content causes blockage of the blood flow of the small vessels. The head of the femur is particularly susceptible due to precarious blood supply.
Another effect of glucocorticoids is high blood pressure in the body. Constant hypertension causes the narrowing of the small blood vessels of the body. The arteries in the head of the femur constrict leading to a reduction in the blood supply of the head.
The reduced blood supply and blockage of the venous supply causes increased pressure build-up in the head of the femur. The bone cells deprived of their nutrition and oxygen supply die. The head of the femur collapses leading to small fractures in the ball.
The osteoblasts are cells in the bone required for laying down new bone. The osteoblasts also are responsible for releasing factors required for the function of the osteoclasts. The osteoclasts are the cells responsible for the absorption of the bone normally.
In a healthy bone, there is a fine balance between the action of these two types of cells. The balance is lost under the effect of long term glucocorticoid use. The result is cell death in the bone.
The spherical contour of the head of the femur is lost. The incongruity causes grinding of the joint surface leading to arthritic changes. In the end stages, the bone collapses and the joint becomes severely arthritic and loses the function.
The symptoms of AVN hip is joint pain and stiffness. The patients may walk with a limp. Some of the patients may experience a restriction of movements in one direction. The restriction gradually becomes global leading to fixation of the hip in one position.
The diagnosis of avascular necrosis of the hip is made by a physician after a thorough physical examination and radiological evidence. The physician looks for tender points and moves the hip through a range of motion. The restriction of motion of the hip in various planes is examined.
Both the hips are usually involved in the case of high dose steroid-induced avascular necrosis. The imaging tests are done in the form of an X-ray and MRI. The X-ray might show the areas of the collapse of the head of the femur. An X-ray also provides information about the arthritic changes in the ball and the cup of the joint.
By the time the changes of avascular necrosis are evident on an X-ray, the AVN is in advanced stages. An MRI and bone scan are able to detect changes in the early stages of the disease. The necrosis of bone in the early stages is evident as signal changes in an MRI.
The Management of avascular necrosis usually depends upon the stage of the disease. A vast majority of the avascular necrosis patients usually present in the late stages. A total hip joint replacement offers an excellent treatment in such cases.
Other management options include the use of core decompression and stem cell therapy. The core decompression technique involves the use of small drills made in the head of the femur. The pressure inside the head of the femur is reduced allowing revascularization and repair.
Stem cell therapies involve the use of stem cells cultured to be inserted in the necrotic parts. The stem cells have the potential to turn into bone cells and allow repair of the necrotic segments.
Some of the other techniques used are surgical dislocation of the hip joint and removal of the necrotic segment and graft insertion. Various bone cutting and rotational surgeries known as rotational osteotomies may be used in the early stages.
Currently, there is limited evidence of the effectiveness of these techniques in the treatment of avascular necrosis of the hip. Total hip replacement remains the best surgical treatment option for these patients.
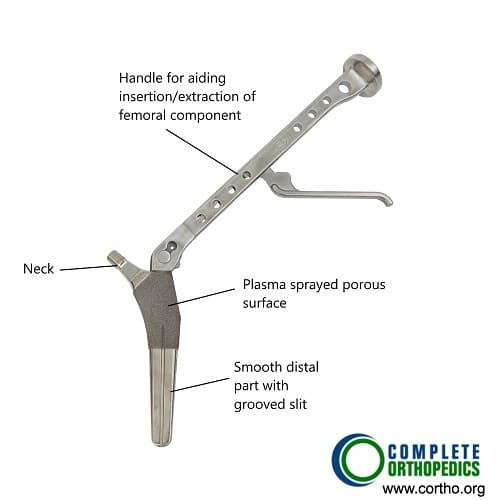
Femoral Component in Primary Hip Replacement
The image shows a femoral component used in primary hip replacement. The metallic implant has a plasma porous coated layer in the upper part. The plasma coated layer aids in bone ingrowth on the implant for a steadier fixation. The lower part is smooth for aiding insertion and has grooved slit to allow blood and debris to come out while insertion in the canal.
Total hip replacement of the hip joint offers early relief from pain and return to previous activity. With the advancement of surgical techniques and instruments, a successful total hip replacement may last for 15-20 years or even more.
Do you have more questions?
Are there any alternative treatment options for managing the underlying medical condition for which I require cortisone therapy, which may carry a lower risk of avascular necrosis?
Depending on the specific medical condition, there may be alternative treatment options available that carry a lower risk of avascular necrosis. These may include nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), physical therapy, lifestyle modifications, or surgical interventions. It’s essential to discuss these options with your healthcare provider to determine the most appropriate course of treatment for your individual circumstances.
What should I do if I experience new or worsening joint symptoms while on cortisone therapy, and how quickly should I seek medical attention?
If you experience new or worsening joint symptoms such as pain, stiffness, or decreased range of motion while on cortisone therapy, it’s important to promptly inform your healthcare provider. Depending on the severity of symptoms, they may recommend further evaluation, adjustments to cortisone dosage, or additional treatments.
Are there any lifestyle modifications or precautions I should take if I’m on cortisone therapy to minimize my risk of developing avascular necrosis?
Yes, maintaining a healthy lifestyle is crucial. This includes regular weight-bearing exercise to promote bone health, a balanced diet rich in calcium and vitamin D, avoiding excessive alcohol consumption, and cessation of smoking. Additionally, patients should follow their healthcare provider’s recommendations for cortisone use closely.
Can avascular necrosis occur in patients who have been prescribed cortisone for short-term use, such as for acute conditions or injuries?
Avascular necrosis can occur even with short-term cortisone use, although it’s less common compared to long-term use. However, patients should be monitored for symptoms, especially if they have other risk factors such as pre-existing joint disease or previous cortisone use.
Is there a specific threshold or cumulative dose of cortisone beyond which the risk of developing avascular necrosis significantly increases?
While there is no precise threshold or cumulative dose established, higher doses and prolonged use of cortisone increase the risk of avascular necrosis. Individual susceptibility factors also play a significant role. Therefore, it’s essential to use cortisone judiciously, balancing its benefits with the potential risks.
How important is it for patients on cortisone therapy to undergo regular monitoring and screening for avascular necrosis, and at what intervals should these assessments be performed?
Regular monitoring and screening for avascular necrosis are essential for patients on cortisone therapy, particularly those at higher risk due to factors such as prolonged or high-dose cortisone use. Your healthcare provider can recommend an appropriate schedule for monitoring based on your individual risk factors and medical history.
Are there any alternative treatments or medications that can be used to manage avascular necrosis in patients who need to continue cortisone therapy?
While total hip replacement remains the gold standard treatment for advanced avascular necrosis, other conservative measures such as pain management, physical therapy, and lifestyle modifications may help alleviate symptoms and slow disease progression. Your healthcare provider can help develop a comprehensive treatment plan tailored to your individual needs and circumstances.
If avascular necrosis is diagnosed while on cortisone therapy, can discontinuing the cortisone treatment help slow or halt the progression of the condition?
Discontinuing or tapering cortisone therapy may be considered as part of the treatment plan for avascular necrosis, especially if the cortisone use is identified as a contributing factor. However, this decision should be made in consultation with your healthcare provider, taking into account the underlying medical condition and potential risks of stopping cortisone therapy abruptly.
Are there any additional precautions or monitoring measures I should take if I’m on long-term cortisone therapy to reduce my risk of avascular necrosis?
In addition to regular monitoring by your healthcare provider, it’s essential to maintain a healthy lifestyle, including regular exercise and a balanced diet, to support overall bone health. Your healthcare provider may also recommend bone density testing or other screening measures to assess your risk of developing avascular necrosis.
Can avascular necrosis progress rapidly once it starts, especially in patients on cortisone therapy?
Avascular necrosis can progress at varying rates depending on individual factors such as the underlying cause, severity of cortisone use, and overall health. In some cases, avascular necrosis may progress rapidly, particularly if not identified and managed early.
Are there any signs or symptoms that indicate I may be developing avascular necrosis while on cortisone therapy?
Symptoms such as persistent joint pain, stiffness, or difficulty bearing weight on the affected joint may indicate the development of avascular necrosis. It’s important to promptly report any new or worsening symptoms to your healthcare provider for evaluation.
Can avascular necrosis occur after receiving cortisone injections directly into the affected joint?
While less common than with systemic corticosteroid use, avascular necrosis can still occur as a complication of cortisone injections, especially when administered repeatedly or in high doses. It’s essential to discuss the potential risks and benefits of cortisone injections with your healthcare provider.
What are the potential complications or risks associated with total hip replacement surgery?
Potential complications of total hip replacement surgery include infection, blood clots, dislocation of the implant, implant wear or loosening over time, nerve injury, and leg length discrepancy. Your surgeon will discuss these risks with you in detail before the procedure.
Are there any support groups or resources available for people dealing with avascular necrosis?
Yes, there are support groups and resources available for individuals dealing with avascular necrosis. These may include online forums, local support groups, and educational materials provided by organizations such as the Arthritis Foundation and the National Osteonecrosis Foundation. Your healthcare provider can help you access these resources.
How successful is total hip replacement in relieving pain and restoring mobility for patients with avascular necrosis?
Total hip replacement is highly successful in relieving pain and restoring mobility for patients with avascular necrosis. The procedure involves replacing the damaged hip joint with an artificial implant, which can significantly improve quality of life for individuals with this condition.
If I develop avascular necrosis, what are the chances that I’ll need a total hip replacement?
The likelihood of needing a total hip replacement for avascular necrosis depends on factors such as the severity of the condition, the extent of joint damage, and your overall health. Your healthcare provider will evaluate these factors and discuss the most appropriate treatment options for you.
Are there any dietary changes or supplements that may help prevent avascular necrosis?
While there are no specific dietary changes or supplements proven to prevent avascular necrosis, maintaining a balanced diet rich in calcium and vitamin D can support overall bone health. However, it’s essential to consult with your healthcare provider before starting any new dietary supplements.
How often should I have imaging tests like X-rays or MRIs to monitor for avascular necrosis if I’m on long-term corticosteroid therapy?
The frequency of imaging tests such as X-rays or MRIs for monitoring avascular necrosis depends on various factors, including the duration of corticosteroid therapy and the presence of symptoms. Your healthcare provider will recommend the appropriate imaging schedule based on your individual circumstances.
Are there any warning signs or symptoms of avascular necrosis that I should watch out for?
Common warning signs and symptoms of avascular necrosis include joint pain, stiffness, limited range of motion, and difficulty walking. If you experience any of these symptoms, it’s important to consult with your healthcare provider for further evaluation.
What lifestyle changes can I make to reduce my risk of avascular necrosis if I need to continue taking corticosteroids?
Lifestyle changes that can help reduce the risk of avascular necrosis include maintaining a healthy weight, avoiding excessive alcohol consumption, avoiding smoking, and engaging in regular physical activity. It’s also important to follow your healthcare provider’s recommendations regarding corticosteroid use.
Can avascular necrosis occur in other joints besides the hip?
Yes, avascular necrosis can occur in other joints besides the hip, such as the knee, shoulder, and ankle. However, the hip is the most commonly affected joint, especially in cases related to corticosteroid use.
Are there any alternative medications or treatments that can be used to manage my condition without increasing the risk of avascular necrosis?
There are alternative medications and treatments available for managing various conditions without the risk of avascular necrosis. These options depend on the specific medical condition being treated and should be discussed with your healthcare provider.
How long does it typically take for avascular necrosis to develop after starting corticosteroid treatment?
Avascular necrosis (AVN) can develop within a few months to several years after starting corticosteroid treatment. The duration varies depending on factors such as the dosage and duration of corticosteroid use, as well as individual predisposing factors.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
