Case Study: Knee Arthroscopy: Medial Meniscectomy
with Femoral Chondroplasty in a 60 year-old guy
The patient is a 60-year-old guy who has seen a doctor several times for pain on the inner side of his left knee, as well as buckling and giving way. We performed an MRI, which revealed a medial meniscus rupture as well as a partial high-grade ACL tear.
We examined treatment alternatives and decided on surgical intervention. We reviewed the dangers and benefits of infection, hemorrhage, nerve and artery injury, re-surgery, rehabilitation, further arthritis progression, and future knee replacement, among other things.
We talked about systemic concerns such as blood clots, cardiac, pulmonary, and neurological issues. We also explained how, given his age, the barrier for performing an ACL reconstruction would be high. The patient comprehended and signed an informed consent form.
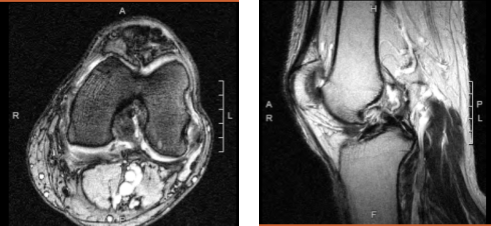
Magnetic resonance imaging of the left knee
The patient was brought into the operation room and placed on a well-padded operating table. Anesthesia was administered. A tourniquet was wrapped around the patient’s left thigh. It was secured in a holder. As is customary, the left knee was prepped and draped aseptically. A timeout was issued. A preoperative antibiotic was administered.
To insert the arthroscope, a lateral entry hole was created. A spinal needle was used to create a medial entrance hole. The patellofemoral compartment revealed no osteoarthritic alterations.
A lateral free edge and inferior and horizontal tearing in the posterior horn of the medial meniscus were found, as well as grade 2 to 3 osteoarthritic alterations in the medial femoral condyle with loose flaps. Debridement of the meniscus and cartilage was performed with a shaver and biters.
Balanced margin was achieved. Examination of the intercondylar notch showed partial tearing of the ACL with intact footprint over the femur as well as tibia. It was decided not to do ACL reconstruction. Examination of the lateral tibiofemoral compartment showed intact meniscus and cartilage.
The knee was thoroughly irrigated and drained. Final pictures were taken and saved. Closure was done with 3-0 nylon. Then, 50 mL of 0.258 Marcaine mixed with 40 mg of Depo-Medrol was injected into the knee. Dressing was done with the use of Adaptic, 4×4, ABD, Webril, and Ace wrap.
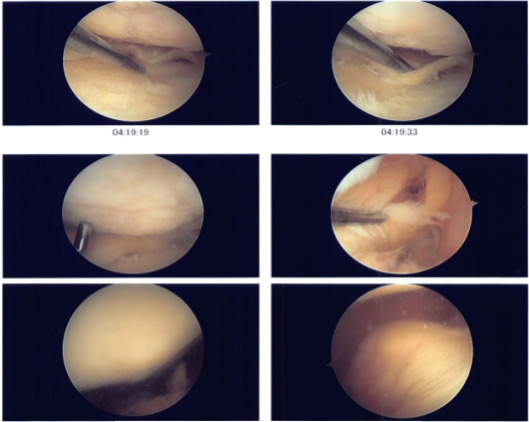
Intraoperative photo
The patient was extubated and moved to recovery in a stable condition. The patient seen in the office for his postoperative visit. He is not improving in his pain in the left knee.
We opted to proceed with official physical therapy as well as a home workout regimen for knee rehabilitation after examining treatment choices. During the visit, we reviewed the arthroscopy images and removed the stitches. We will continue to use ice and elevate the knee to reduce swelling and pain.
To limit the risk of deep vein thrombosis, we will continue to use early mobilization and mechanical prophylaxis. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress. The patient is seen in the office every four weeks if his follow up visits and physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
