Case Study: Left Knee Arthroscopy: Chondroplasty
and Microfracture in a 30 year-old patient
The purpose of this operation is to stop or delay additional cartilage deterioration. By doing this, knee arthritis can be avoided. It may enable you to put off the requirement for a partial or complete knee replacement. Additionally, this process is utilized to relieve knee discomfort brought on by cartilage damage.
Rarely do knee pain symptoms indicate a disease that might be fatal. Deep vein thrombosis, a blood clot that can migrate up your leg and into your lung, is a disorder that, in rare instances, needs prompt emergency care.
For associated symptoms, weakness and pain with motion but reports no numbness, no tingling, no swelling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness.
The patient presented MRI thaw showed full-thickness cartilage fissure trochlea with underlying subchondral bone marrow edema and small subchondral cysts.
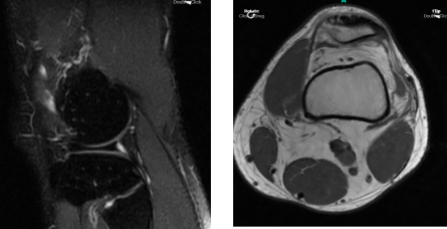
MRI Left Knee Non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and I think that is a reasonable option. I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery. The patient expressed understanding of these risks and has elected to proceed with surgery.
I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room after a due informed consent. The left knee was prepped and draped aseptically in the usual fashion. Antibiotics were given. Tourniquet was elevated. was called. A lateral entry portal was made. Arthroscope was inserted.
A medical entry portal was made with the aid of a spinal needle. Shaver was inserted to clean the debris. Examination of the medial tibiofemoral compartment showed intact meniscus and cartilage. Examination of the intercondylar notch showed synovitis in the region of the ACL and the intercondylar notch.
This was repeated with the use of a shaver and followed by Coblation to take care of hemostasis. Examination of the lateral tibiofemoral compartment showed intact cartilage and meniscus. Examination of the patellofemoral compartment showed focal loosening of the cartilage flap, which was debrided with the use of shaver.
It was found that bone was exposed, and it was a grade 4 lesion. All the loose cartilage was removed with the use of a shaver followed by a Coblation wand. The wound was exposed. The lesion was less than 0.5 mm x 0.5 mm, so the decision was done to do a microfracture chondroplasty.
Chondral pick set was used and chondral picks were used with the help of a hammer and three holes were made into the bone. Shaver was used to clean up the margins. The knee was thoroughly irrigated and drained.
Closure was done with nylon #3-0. Then, 20 cc of 0.5% Marcaine mixed with 40 mg of Depo-Medrol was injected into the knee. Dressing was done with the use of Adaptic, 4 x 4, ABD, Webril, and Ace wrap. The patient was extubated and moved to recover in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
