Case Study: Knee Arthroscopy: Pain in right knee
Chondroplasty in a 40 year-old male
Chondroplasty is a procedure that involves smoothing degenerative cartilage and reducing unstable cartilage flaps in order to stabilize and treat chondral lesions. Trimming unstable flaps of a torn meniscus to create a stable remnant meniscus is what partial meniscectomy entails.
Chondroplasty is a minimally invasive surgical method for repairing damaged knee cartilage. A surgeon uses arthroscopic technology to remove damaged tissue from the joint and assist handle any future issues. When diseased tissue is removed, healthy cartilage can develop in its place.
Chondroplasty is a minimally invasive surgical method for repairing damaged knee cartilage. A surgeon uses arthroscopic technology to remove damaged tissue from the joint and assist handle any future issues. Arthroscopic chondroplasty is a frequent surgical treatment performed during knee arthroscopy.
Specifically, chondroplasty is used to smooth damaged cartilage in the knee in order to reduce joint friction. It is a possibility for people who have mild to severe cartilage wear. Though you may require crutches or other help following chondroplasty, you should be able to resume normal activities within three weeks.
The patient is a 40-year-old male who came into the office after being involved in a car accident. He attempted conservative care, such as physical therapy and anti-inflammatory drugs, but these were ineffective. An MRI revealed an osteochondral defect of the lateral femoral condyle.
We examined treatment alternatives and decided on surgical intervention. We reviewed risks and benefits such as infection, hemorrhage, nerve and artery injury, rehabilitation, and the necessity for repeat surgery, among other things. We talked about systemic concerns such as blood clots, cardiac, pulmonary, and neurological issues. The patient comprehended and signed an informed consent form.
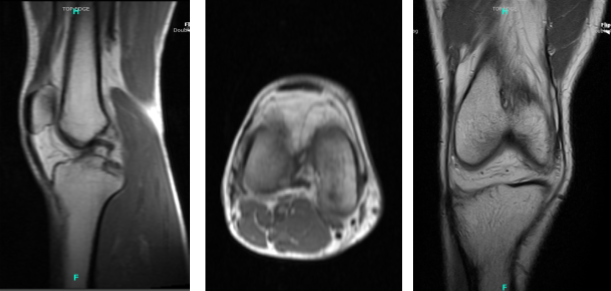
MRI Right knee non-contrast
The patient was transported to the operating room, where he was given general anesthesia. A tourniquet was placed around the lower thigh. The patient was placed on a well-padded bed, and the thigh was clamped. As is customary, the right knee was prepped and draped aseptically. Antibiotics were administered before the surgery. The tourniquet had been inflated. A timeout was issued.
An incision with a blade was used to create a lateral entry portal, and the arthroscope was inserted. The patellofemoral compartment revealed intact cartilage over the patella.
A grade 1 to grade 2 osteochondral lesion of the medial femoral condyle was discovered during an examination of the medial tibiofemoral compartment. A spinal needle and blade were used to create a medial entrance hole. The osteochondral lesion was debrided to stable margins using a shaver.
Further inspection revealed neither medial or lateral meniscus tears. The ACL was not torn. A thorough inspection of the lateral femoral condyle revealed no free cartilage fragments. The osteochondral lesion appeared to be stable and was left alone.
The patellofemoral compartment was examined again and revealed several grade 1 osteochondral lesions of the trochlea, which were left alone. Photographs were taken and preserved. The knee was irrigated and drained extensively.
The arthroscope was withdrawn, and the wound was closed with nylon. The knee was then injected with 20 mL of 0.5% Marcaine combined with 40 mg of Depo-Medrol. Xeroform, 4×4, ABD, Webril, and Ace Wrap were used in the dressing. In stable condition, the patient was extubated and transported to recovery.
After one week the patient is here for his postoperative visit, no X-ray needed. We talked about therapy options such as physical therapy, MRI, injections, and surgery. We agreed to practice conservative management for the time being. PT will continue, as will the use of ice and elevation, as well as the use of over-the-counter anti-inflammatory drugs and pain relievers. There will be another checkup in four weeks.
Months later, the patient visits the office for his postoperative visit, no X Ray needed. He has pain going up and down the stairs. We discussed therapy alternatives such as PT, MRI, injection, and surgery.
We agreed to use conservative management for the time being. PT will continue, as will the use of ice and elevation, as well as the use of over-the-counter anti-inflammatory medications and after 4 weeks, there will be another checkup. The patient is still making improvement, albeit slowly, with help of monthly examinations and physical treatment and at home.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.