Case Study: Arthroscopic Debridement, Decompression
Acromioplasty and Distal Clavicle Excision of the left shoulder
Human shoulder is known as the most extensive range of motion in the human body. Our muscles in our shoulders help us to abduct, adduct, flex, extend and rotate.
Based on research, there are three common injuries on the human shoulder: instability, frozen shoulder and the popular is rotator cuff tear. In this article, rotator cuff tears will be tackled. Without treatment, rotator cuff tear may lead to permanent loss of motion.
Patient is in our office, with complaints of shoulder. The pain started over a week ago. The patient remembers an injury in a fall, where her right foot got caught in concrete and tripped. Patient had gone to the ER afterwards.
The pain is associated with swelling, bruising, numbness, tingling, and radiating pain. The pain is getting worse from the day it started. We have been treating the left shoulder conservatively but no relief.
Upon examination of the cervical spine, the patient is tender to palpation over the paraspinal musculature. They are nontender over the spinous processes and have no crepitus with range. There is limited range of motion of the spine due to discomfort. They have a negative Spurling’s test.
They sit with the scapular protracted and depressed. They are tender to palpation over the trapezius and rhomboids. They are nontender to palpation over the clavicle and elbow. There is no soft tissue swelling or ecchymosis.
The patient has a full range of motion of the shoulders. The shoulders are stable on exams. They have 5/5 strength, and are neurovascularly intact distally. There are no erythema, warmth, or skin lesions present.
Left shoulder X Ray were presented and discussed and showed normal left shoulder radiographs. Recommended patient to undergo MRI to see the reason behind the pain. Found that there is very minimal AC joint osteoarthritis. No subacromial enthesophyte is visualized. Also noticed, mild rotator cuff tendinosis.
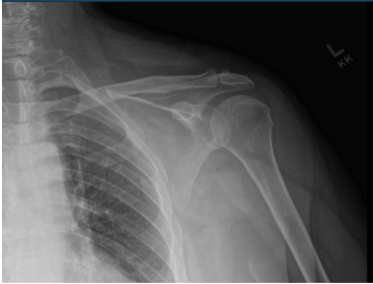
Left Shoulder X-ray
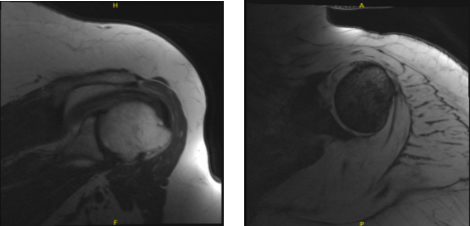
MRI-3T Left Shoulder Non-contrast
Patient opted for surgical management.
We discussed risks and benefits of surgery, including infection, nonhealing, need for repair, rehabilitation, possibility of decreased suboptimal result, need for repeat surgery, need for rehabilitation and physical therapy, need for cortisone injection in the future, systemic problems including injury to adjacent nerves and vessels; systemic problems including blood clot, cardiac, neurological, pulmonary complications and even death.
The patient understood and signed an informed consent.
The patient was taken to the operating room where a brachial block was given. General anesthesia was induced. The patient was put in a lateral position with the left shoulder up. Positioning was held by a beanbag and all the bony prominences were well padded.
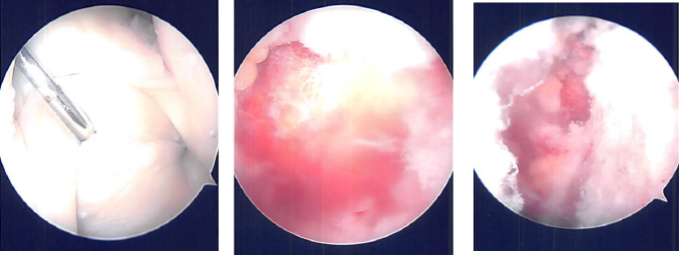
Surgical incision was given behind the posterolateral corner of the acromion. The scope was entered into the glenohumeral joint. Examination of the glenohumeral joint was performed. There was a labral hole. There were labral degenerations, which were shaved.
There was degeneration of the posterior labrum which was cleaned with shaving. Subacromial bursitis was present. The thorough bursectomy was done using a shaver. A lateral portal was made. There was fraying of the acromion along with a curved configuration (type 2) was present.
Decision of acromioplasty was taken. Acromioplasty was performed after cleaning with a thermal wand and then followed by a bur. After a thorough acromioplasty, the AC joint was examined and found to be having degeneration. The distal clavicle excision was planned. The distal clavicle excision was done using a wand followed by bur.
About a centimeter of distal clavicle was excised. Final pictures were taken and saved. Closure was done using Nylon #4-0. The patient was extubated and moved to the recovery unit. Dressing was performed using Adaptic, 4 x 4, ABD, tape. The patient’s shoulder was put in a shoulder immobilizer.
After a week post-operative, a patient came into the office to discuss the treatment options. We have decided to proceed with formal physical therapy as well as a home exercise program for the rehabilitation of her shoulder.
Stitches were removed. Patient will continue the ice and elevation for it helps on her condition. The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
