Case Study: Knee Arthroscopy: Patellofemoral Chondroplasty
and Partial Medial Meniscectomy in a 45 year-old male
An essential diagnostic and treatment aid for the management of knee disorders is knee arthroscopy. Meniscectomy, loose body removal, chondroplasty, microfracture, irrigation and debridement, and tendon reconstruction are examples of indications. In this set of articles, we provide an in-depth analysis of Patellofemoral Chondroplasty and Partial Medial Meniscectomy.
Chondroplasty refers to the smoothing of degenerative cartilage and trimming of unstable cartilage flaps to stabilize and treat chondral lesions. Partial meniscectomy involves trimming unstable flaps of a torn meniscus to establish a stable remnant meniscus.
A 45-year-old male examined with complaints of the left knee. He is a skilled worker who is on his feet for most part of his work. He states he participates in rigorous training and that might have played a part in the injury he sustained. The pain was mild, but it has gotten progressively worse and has been associated with limp. Also, patients complain of clicking on movement.
Upon examination of the left knee, the patient is tender to palpation along the medial joint line, and has an effusion. The patient has discomfort with McMurray’s maneuvers, (the McMurray test is a series of knee and leg movements used to diagnose a torn meniscus) and the knee is stable.
They lack full flexion secondary to the effusion, but have full extension. They have 5/5 strength, and are neurovascularly intact distally. There are no erythema, warmth or skin lesions present. On examination of the contralateral extremity, the patient is nontender to palpation and has excellent range of motion, stability and strength.
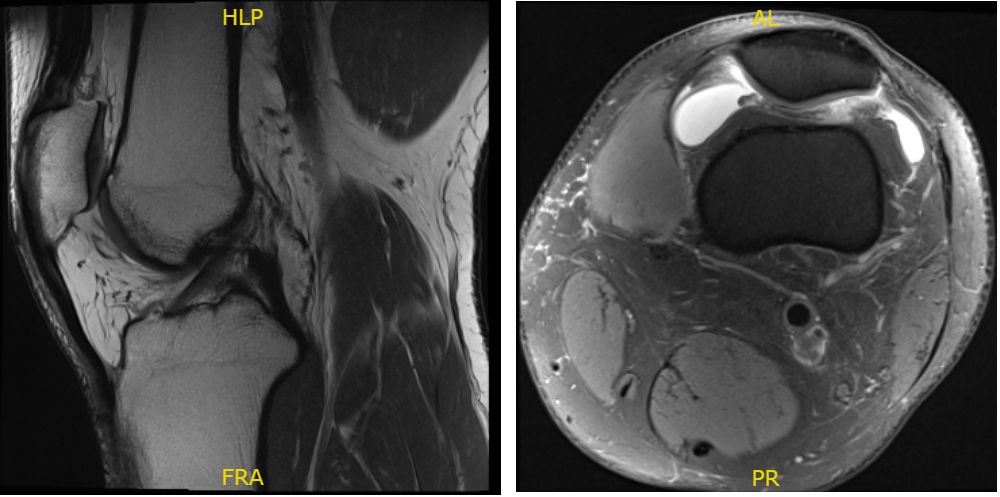
Fig. 1 MRI of the left knee in sagittal and coronal sections.
There is no acute fracture or osteonecrosis however there is mild patellofemoral compartment cartilage wear and a complex tear of the medial meniscus involving the body and posterior horn.
There is a focal full-thickness cartilage fissuring overlying the lateral trochlea with mild reactive subchondral edema. The tear demonstrates a predominant longitudinal component within the posterior horn. Additional horizontal oblique tearing is noted with free edge margin fraying.
Mild reactive edema is present within the subjacent medial tibial plateau. The posterior root attachment is intact. There are no full-thickness cartilage defects. There is a moderate joint effusion. A very small popliteal cyst is present. There are no intra-articular ossific loose bodies.
We talked about conservative versus operative management of her current pain pattern. The patient understands that there is no guarantee that arthroscopy is going to get rid of all of his pain.
He understands that there may be a possibility in which the pain is only minimally reduced. We discussed risks, benefits, and complications of the treatment. The risks, benefits, alternatives, and complications were discussed with the patient at length.
We discussed infection, bleeding, injury to nerves and vessels, knee pain, swelling, the progression of arthritis, the need for cortisone injections in the future and the need for rehabilitation. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure. The patient understood and signed informed consent.
An arthroscopic surgery was performed. The probe was inserted on the medial portal and the posterior horn of the medial meniscus was examined. It showed a complex tear up to tie periphery.
There were degenerative changes in the meniscus with calcification. The tear was not repairable. A decision for meniscectomy was taken and the meniscus was debrided and cleaned up to the stable edges using shaver and punch.
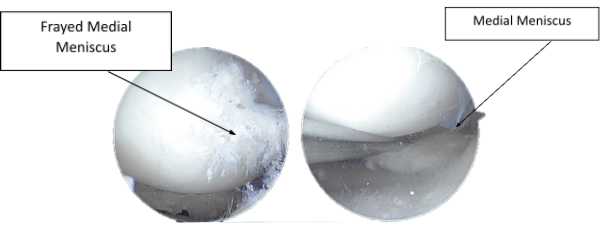
Figure 2.1. Intraoperative Arthroscopy Images
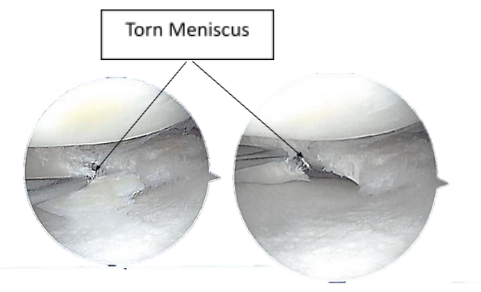
Figure 2.2. Intraoperative Arthroscopy Images

Figure 2.3 Arthroscopic view tear of the lateral meniscus posterior horn
Debridement of the cartilage was performed to remove the loose edges. Grade 2 to grade 3 OA lesions were also found on the trochlea, where debridement of the cartilage was performed. The chondroplasty was performed to remove the free edges.
The medial and lateral gutters were examined. Here was no loose body. The scope was changed from the lateral to medial portal and further chondroplasty of the patellofemoral joint, as performed. The medial meniscus was examined and found to be stable.
Final arthroscopic pictures were taken and saved. The knee was washed with copious saline and scope was removed. The incision was cleansed with nylon 3-0 and dressing was done with Adaptic, 4 x 4 and BD followed by Webril and Ace wrap.
The tourniquet was removed. The count was complete at the end of the procedure. The patient was extubated and moved to the stretcher and into the postoperative care unit.
After a week of seeing patients, he has been improving with regards to pain and swelling. He is limping and has been using crutches for ambulation. Denies fever, chills, reinjury. After two weeks post surgery the incisions are healing well, without evidence of drainage, erythema or warmth.
There is a full range of motion without discomfort. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
