Case Study: Knee Arthroscopy: Partial Medial
or Lateral Meniscectomy in a 40 year-old female
Parts of a symptomatic, torn meniscus are removed during a partial meniscectomy, a minimally invasive outpatient operation, using an arthroscopic and small arthroscopic tools. On the inside of the knee joint is the medial meniscus.
On the outside of the knee is the lateral meniscus. Size and severity of meniscus tears can vary significantly. A meniscus might be torn in half, have a C-shaped rip around its perimeter, or be left attached by a thread to the knee joint.
A 40 year-old female patient visits the office with the complaints in her right knee pain due to a motor vehicle accident that occurred a few months ago. She had no pain in her neck, back or right knee prior to the accident.
She has tried PT with no relief, she smokes but plans to quit and is a mother of 5. MRI was performed which showed a tear of lateral meniscus but before that she was seen in the office for the last few months, and got surgery because of medial meniscectomy on the right knee that she experienced more than three months back.
The patient had a “twisting injury” in that post op rehab period and injured the knee again. She was complaining of worsening her right knee.
The doctor reviewed and discussed the diagnosis, there is increasing volume of synovial fluid extending primarily medially from the level of the patellofemoral articulation and outlines the medial patellofemoral plica.
There is Hoffa’s fat pad scar related to interval arthroscopic surgery that has occurred since the previous study. There is a new obliquely oriented fairly peripheral tear involving the body and body-anterior horn junction of the lateral meniscus extending at the peripheral third of the meniscus.
The medial meniscus again demonstrates free edge truncation and radial tearing versus postoperative debridement changes involving the body and body-anterior horn junction with small remnant at the medial meniscal body mostly extruded outside the confines of the medial tibiofemoral joint compartment.
There has been a slight increase in medial tibiofemoral joint space narrowing since the previous study. There is again thickening and strain of the medial collateral ligament at its femoral attachment site without appreciable change.
There is again edema in the prepatellar subcutaneous tissues. Osseous signals and morphology are, otherwise, unremarkable. The lateral collateral ligaments, the anterior and posterior cruciate ligaments, quadriceps and patellar tendons are, otherwise, unremarkable.
Increasing volume of synovial fluid extends primarily medially from the level of the patellofemoral articulation and outlines the medial patellofemoral plica. Hoffa’s fat pad scar is related to interval arthroscopic surgery that has occurred since the previous study.
New obliquely oriented fairly peripheral tear involving the body and body-anterior horn junction of the lateral meniscus extending at the peripheral third of the meniscus.
The medial meniscus again demonstrates free edge truncation and radial tearing versus postoperative debridement changes involving the body and body-anterior horn junction with small remnant at the medial meniscal body mostly extruded outside the confines of the medial tibiofemoral joint compartment. There has been a slight increase in medial tibiofemoral joint space narrowing since the previous study.
Thickening and strain of the medial collateral ligament at its femoral attachment site without appreciable change. Edema in the prepatellar subcutaneous tissues.
The doctor started to discuss the treatment options, the patient tried conservative management, but she failed. The patient opted for surgical management. We discussed risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, rehabilitation, failure of surgery, need for repeat surgery, arthritis, need for total knee replacement in the future among others.
We also discussed systemic complications including blood clots, cardiac, pulmonary, neurological complications including death. The patient understood and signed the informed consent.
The patient was taken to the operating room area where she was placed on a well-padded operating room table. General anesthesia was induced. Tourniquet was applied. Preoperative antibiotic was given. The right lower extremity was prepped and draped aseptically in the usual sterile fashion.
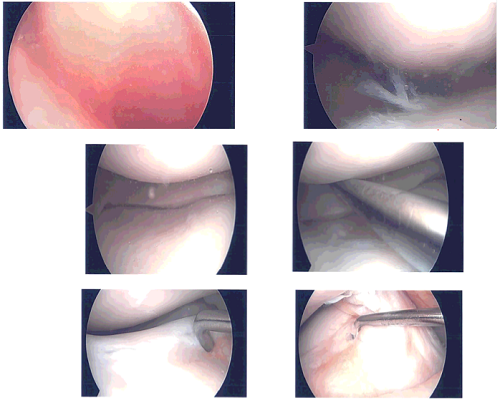
Time-out was called. A lateral entry portal was made. Arthroscopic was inserted and a medial entry portal was made for entry of the instruments. Examination showed a lateral margin fraying of the medial meniscus which was debrided with the use of shaver and Coblation wand.
There was no arthritis of the medial tibiofemoral compartment. Examination of the intercondylar region showed intact ACL. Examination of the lateral tibiofemoral compartment showed tear in the anterior horn of the lateral meniscus, which was debrided with the use of shaver and Coblation wand.
There were no arthritic changes. Examination of the patellofemoral compartment showed grade 1 to grade 2 arthritic changes in the patella, which was cleaned with the Coblation wand. Superior plica was found to be inflamed and was excised with the use of Coblation wand and shaver. Finally, pictures were taken and saved.
The knee was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon. Then 9 cc of Nar opin mixed with 1 mg of Depo-Medrol was injected into the knee. Dressing was done with the use of Xeroform, 4 x 8s, ABD, Webril, and Ace wrap. The patient was extubated and moved to recovery in a stable condition.
Integumentary photography, whole body
After two weeks the patient is seen in the office for her post operative visits, no x rays are needed. She denies pain, chills, she has some drainage from the knee which has stopped and she is ambulating with limp without aid.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain.
We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis. We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications. With regular visits in the office, the patient did well after the surgery and continued physical therapy for the knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.