Case Study: Left Knee Medial Patellofemoral
Ligament Reconstruction in a 21 year-old patient
To support the knee and aid in preventing further injury to the joint, an MPFL reconstruction involves the creation of a new medial patellofemoral ligament. The MPFL is most commonly injured during lateral patellar dislocation.
This typically occurs when the foot is planted and an internal rotatory force is applied to the flexed knee in the valgus. It is the most important structure that is injured in cases of acute dislocation of the patella.
A 21-year-old patient was in our office with complaints regarding left knee pain due to falling. She has recurrence of dislocation of the kneecap which has been becoming more frequent. She is not able to bear weight and is in knee immobilizer and on crutches.
For aggravating factors, standing, walking, weight bearing, exercise, upstairs, and downstairs. For associated symptoms, tender to the touch. For quality, she reported frequently and constantly. For severity, mild.
For timing, she reported chronic and nighttime weather. For alleviating factors, ice, and rest. For previous surgery, none. For previous injections, she reportedly helped a little. The patient presented X Ray results that showed small right knee joint effusion. Otherwise unremarkable right knee radiographs.
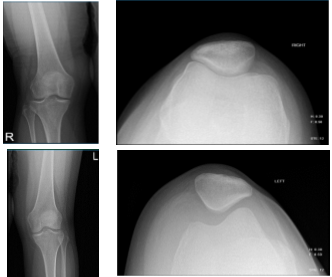
Knee X-ray complete with patella
The patient also presented an MRI result that showed findings in keeping with recent transient lateral patellar dislocation with impaction contusions of the inferomedial patella and anterolateral distal femur. Partial tearing at the patellar attachment of the medial retinaculum. Moderate joint effusion. Partially ruptured popliteal cyst.
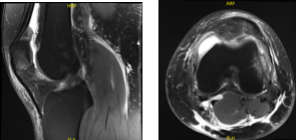
MRI Left Knee non-contrast
We discussed the treatment options for the patient’s diagnosis, which included living with the extremity as it is, organized exercises, medicines, injections and surgical options. I also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
I educated the patient regarding the inherent and unavoidable risks which include, but are not limited to infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
I also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understands there is a long rehabilitative process that typically follows the surgical procedure.
I talked about the possibility of not being able to alleviate all the discomfort. Also, I explained there is no guarantee all the function and strength will return. I discussed the type of implants that may be utilized during this surgery.
The patient expressed understanding of these risks and has elected to proceed with surgery. I discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. I have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome, and post operative protocol.
The patient was taken to the operating room where she was placed on a well-padded operating room table. General anesthesia was induced. Preoperative antibiotics were given. A tourniquet was applied over the left thigh. Left thigh was prepped and draped aseptically in usual fashion. Esmarch was applied.
The knee was kept on a triangle and bony prominences were marked. An incision was given along the medial margin of the proximal patella. With Bovie, the medial margin of the superior patella was dissected clean off its soft tissue footprint.
The capsule was intact. Semitendinosus graft was prepared on the back table with each and whip stitch with a FiberLoop. A drill was used to prepare or the insertion of the graft and into the patella with a SwiveLock 4.75 mm x2.
Two drill holes were made, one at the mid patella and one at the upper quadrant of the patella superiorly. The graft was loaded onto the SwiveLock x2. I inserted it into each hole. A loop was performed. Now a video fluoroscope was brought in to mark the Schottle point.
A Schottle point could be found and an incision was given over the skin. The incision was dissected deep onto the bone. Now, the guide was again used and with multiple attempts a Schottle point could be found through the guide.
Again, the guidewire was drilled into the bone and guided proximally and anteriorly. A layer was dissected between the second and third layer of the knee superficial to the capsule. The graft was passed and found to be a little short. There was no graft, which was longer than 20 cm.
So, another graft will be opened and looped into this graft to extend the length. A FiberLoop was used to stitch the graft into this loop. The graft was put around the guidewire and knee flexion and extension was checked. The graft was found to be in an acceptable position with flexion and extension.
The preparation to fix the graft on the femoral condyle. The Beath pin was passed laterally out and held with a hemostat. Drilling was done over this Beath pin through almost all the mediolateral width of the femur. The sutures of the graft were fed into the Beath pin and the Beath pin was taken out laterally.
Once the graft was in, a nitinol wire was put beside the graft and affixed with a 6 mm x 23 mm Biocomposite screw. Final fixation was checked again and found to be satisfactory. The wound was thoroughly irrigated and drained.
Closure was done in layers using #0 Vicryl, # 2-0 Vicryl and # 3-0 Monocryl. Dressing was done with the use of Xeroform with the use of Steri-Strips, 4 x 8, ABD, Webril and Ace wrap. Knee immobilizer was applied and the patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on her knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
