Case Study: Left Knee Arthroscopic Medial and Lateral
Meniscectomy to 28 year-old Male Involved in a car accident
The following are frequent types of knee injuries sustained in an automobile accident: A direct impact to the kneecap from your steering wheel or dashboard can result in a fracture. The bones around your kneecap, on the other hand, have the potential to break.
Bones can crack or break cleanly, sending shards all over your knee. If you suffer a minor automobile accident knee injury, your doctor will most likely recommend RICE therapy, which stands for rest, ice, compression, and elevation. However, RICE Therapy may not always work for everyone and may necessitate surgical intervention.
Patient came into the office today complaining that the right part of his neck is painful and started like two weeks ago. However, he also complains that his back is hurting but his right knee is extremely in pain. He is 28-years of age and involved in a car accident.
MRI is needed to see significant results why he is in pain. For now, I prescribed anti-inflammatory until the MRI get done. We agreed to continue physical therapy.
After two weeks, an MRI reviewed and showed that the patient has right knee medial meniscus (post horn) with patellofemoral maltracking. We discussed surgical and non-surgical treatment and the patient decided to try conservative medication. Patients will take Percocet and clindamycin.
However, non-surgical treatment failed and he opted to do the surgery. We discussed risks and complications of surgery including infection, bleeding, nonhealing, and need for the repeat surgery, knee arthritis, knee stiffness, adjunct nerves and vessels, cardiac, pulmonary complications including death. The patient understood and signed the informed consent.
The patient was taken to the operating room where general anesthesia was induced. He was placed supine on the table. The right lower extremity was prepped and draped in usual sterile fashion. A time-out was called. Preoperative antibiotic clindamycin was given IV. The tourniquet was inflated.
A lateral entry portal was made and the arthroscope was entered. Examination of the patellofemoral joint showed no damage. The medial gutter showed debris. The scope was moved to the medial tibiofemoral compartment where a small tear in the posterior horn of the medial meniscus could be seen.
A medical entry portal was made with the use of a spinal needle. The probe was entered and tears were confirmed. The tear was removed using upbiting and shaver. The rest of the meniscus was stable. The scope was moved into the intercondylar area where the ACL was intact.
The scope was moved to the lateral tibiofemoral compartment. There was a small tear on the posterior horn of the lateral meniscus. The tear was removed with the use of a shaver. The rest of the meniscus was intact. There was no excess movement of the meniscus.
The cartilage of the medial and lateral femoral condyle was intact. The knee scope was entered into the patellofemoral joint. Examination of the trochlea and posterior surface of circular patella was found to be intact. No arthritic changes could be found. The knee was thoroughly irrigated and drained.
Closure was done using 3-0 nylon. 9 cc of 0.25% Marcaine and 40 mg of Depo-Medrol was injected into the knee. Dressing was done in the form of Xeroform, Webril, ABD, Ace wrap. The patient was also extubated and moved to recovery in a stable condition.
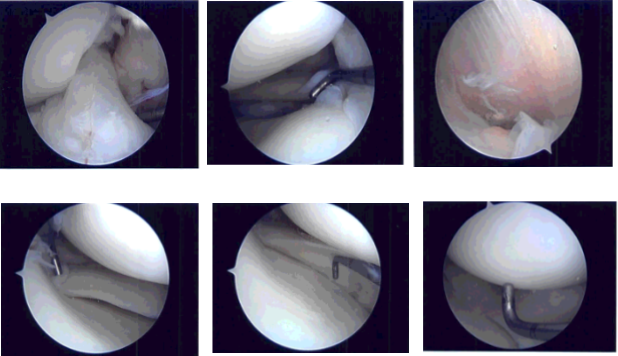
Intraoperative photo
Patient returned after one-week post-operative, pain was well controlled and he denied fever or chills. General Appearance: swelling and tenderness and wound clean and dry, no warmth, appropriate range of motion, and neurovascular intact.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee. We went over the arthroscopic pictures and removed the stitches during today’s visit.
We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications.
We also discussed the risk and benefits and common side effects of taking these medications at today’s visit. I will see them back in three weeks’ time to evaluate their progress. They will call us in the interim if they have any questions or concerns prior to their follow up visit.
By continuing the office visit, and with the help of physical therapy, the patient gets well after the surgery and now back on his normal routine without any pain on his operated knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
