Case Study: Knee Arthroscopy: Patellofemoral Chondroplasty
and Partial Medial Meniscectomy in a 53-year-old male
involved in an automobile accident
A 53-year-old male patient has arrived at our office complaining of lower back, left knee, and left arm pain. The pain began around a week ago.
The patient recalls being injured in an automobile accident. The pain is only moderate in intensity. The pain is continuous and interferes with sleep. The pain is accompanied with numbness.
There is no swelling, bruising, tingling, radiating pain, weakness, bowel or bladder anomaly, gait trouble, giving way, or limping, or difficulty with hand function.
Since its inception, the issue has gotten worse. Walking, bending, and, finally, stairs aggravate the discomfort. Rest alleviates the symptoms. The patient had surgery on his left knee 5 years ago.
Xray were performed on the patient and discussed the result. Left knee Xray showed moderate disc space natto wing medial joint compartment.
Patient has a medial meniscus tear on his left knee. Patient agreed to have an MRI to see further the reason behind the knee pain. Physical therapy also started from the first visit.
After four weeks, the patient returned with the MRI result, mentioned that he has been doing physical therapy 3 times in a week and got no improvement. MRI showed tearing of the medial meniscus at the menisco-capsular junction and posterior horn-body junction. Presence of loss of tricompartmental cartilage and small joint effusion.
We discussed treatment options and opted for surgical management. The patient understands that there is no guarantee that arthroscopy is going to get rid of all of his pain.
He understands that there may be a possibility in which the pain is only minimally reduced. We discussed risks, benefits, and complications of the treatment.
The risks, benefits, alternatives, and complications were discussed with the patient at length. We discussed infection, bleeding, injury to nerves and vessels, knee pain, swelling, the progression of arthritis, the need for cortisone injections in the future and the need for rehabilitation.
The patient also understands there is a long rehabilitative process that typically follows the surgical procedure. The patient understood and signed informed consent.
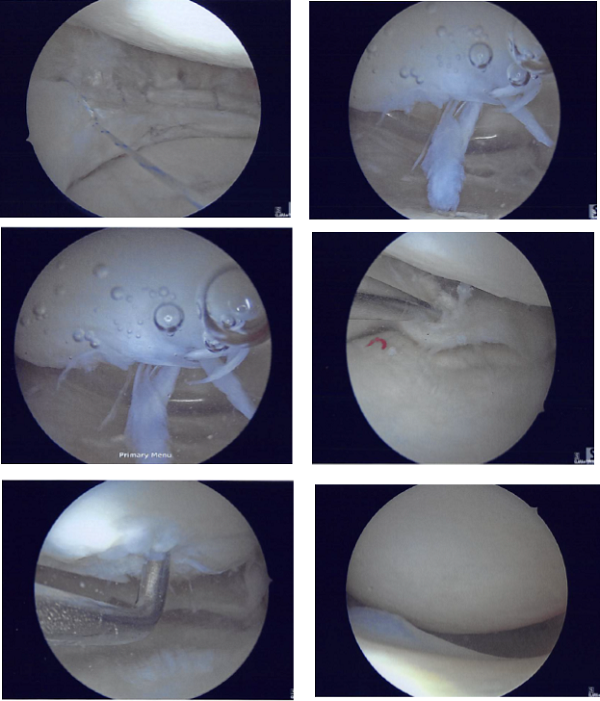
The patient was taken to the operating room, where he was placed on the well-padded operating room table. Left lower extremity was prepped and draped aseptically in usual fashion with a tourniquet applied on the lower thigh. Left lateral entry portal was made. An arthroscope was introduced.
The medial entry portal was made using a spinal needle. Examination of the knee showed OA grade 3 to OA grade 4 arthritis of the trochlea, OA grade 2 to OA grade 3 arthritis of the lateal facet of the patella, OA grade 2 to OA grade 3 arthritis of the medial femoral condyle, previous repair of the medial meniscus because of the sutures as well as long tear of the meniscocapsular junction of the medial meniscus of the left knee.
There was some medial margin tearing and fraying of the lateral meniscus which was taken care with the shaver and meniscectomy performed to stable· margins. The ACL (history of ACL reconstruction) showed fraying in the intertrochlear notch, but the ACL was intact.
Debridement of the ACL was performed. Clean up of the meniscocapsular junction of the medial meniscus was performed. Rasping of the meniscus as well as the capsule was performed in preparation for the repair using shaver and arthroscopic rasps.
Chondroplasty of the medial femoral condyle, trochlea, patellar lateral facet was performed. Decisional for repair was undertaken. All inside repair of the medial meniscus was performed using FasT fixers, five curved, two reversed curved in a sequential fashion.
Following the repair, the meniscus was found to be stable. Final pictures were taken. The knee was thoroughly irrigated. The scope was removed and the knee was drained. The closure was performed with nylon #4-0. Dressing was done using 4x4s, ABD, Webril, and Ace wrap.
The patient returned after a week and he is doing fine and he mentioned that after the surgery his pain improved. He is using a knee immobilizer and not putting weight on his left leg.
After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We removed the stitches during today’s visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
After four weeks post-operative, the incisions are healed well, without evidence of drainage, erythema or warmth. There is a limited range of motion secondary to discomfort (0-90 degrees). There is no calf tenderness.
By this time, the patient wean out of brace, knee immobilizer while ambulating only and he can now drive. The patient regularly followed an office visit every 3-4 weeks. Patient did well after the surgery and continued physical therapy.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
