Case Study: Arthroscopy: Tear of Medial Meniscus
of Knee in a 48 year-old female
An injury to the medial meniscus, a piece of cartilage on the inside (inner aspect) of the knee, is known as a medial meniscus tear. More frequently than lateral meniscus injuries, medial meniscus injuries can cause locking, catching, or buckling as well as pain, stiffness, and edema.
The patient is a 48-year-old female with right knee and right hip pain. She has gained weight recently. She works as a chemist at Este Lauder. After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling.
After a sterile prep, 7cc of 1% Lidocaine and 80mg of depo-Medrol were injected into the right hip trochanteric bursa. The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail.
MRI were reviewed and discussed; Collateral Ligaments: The medial collateral ligament is intact. The lateral collateral ligament, biceps femoris tendon, iliotibial band, and popliteus tendon is intact.
Cruciate Ligaments: The anterior and posterior cruciate ligaments are intact. Menisci: Peripheral oblique tear in the body and posterior horn the medial meniscus. The lateral meniscus is intact. Cartilage: The chondral surfaces in the medial compartment are intact. The chondral surfaces in the lateral compartment are intact.
Focal chondral fissure in the medial patellar facet. Bones: The visualized osseous structures demonstrate normal bone marrow and cortical signal intensity without evidence of fracture, trabecular bone injury or dislocation. No osseous lesions are identified.
Extensor Mechanism: The quadriceps and patellar tendons are normal. Joint: Small joint effusion. The soft tissues are otherwise normal. The neurovascular structures demonstrate normal course. It has an impression: Peripheral oblique tear in the body and posterior horn of the medial meniscus. Focal chondral fissure in the medial patella facet. Small joint effusion.
With the patient, many treatment options, including surgical and nonsurgical treatments, were reviewed. The patient decided to have surgery. We talked about the dangers and benefits, including those related to infection, bleeding, damage to the nerves and blood vessels, stiffness, the requirement for rehabilitation, surgical failure, additional surgery, arthritis, and other issues. Patient signed surgery permission after understanding it.
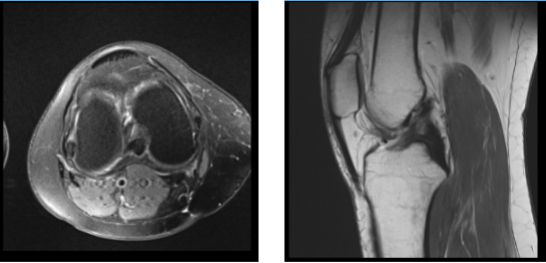
MRI Right Knee Non-contrast
The patient was brought into the operating room and set down on a well-padded operating table. He was given general anesthesia. The patient was unconscious. With the help of 15 cc of 2% Lidocaine combined with.
5% Marcaine and epinephrine, an intra articular block was administered. Right lower extremity was prepared and covered with a drape. It was time for a timeout. Antibiotics were administered before surgery.
A sharp knife was used to make a lateral portal incision. A spinal needle and knife were used to create a medial portal. A vertical, nearly complete rip in Zone 3 surrounding the meniscus’s body was visible upon examination of the medial compartment.
In order to execute a partial meniscectomy, biters and a shaver were used. The medial femoral condyle’s weight-bearing portion had a Grade III to Grade IV lesion, measuring around 1 cm in diameter, according to a cartilage examination.
With the aid of a shaver, this was debrided, and the shaver was then used to execute an abrasion chondroplasty. The infrapatellar notch examination revealed an undamaged ACL. The meniscus and cartilage in the lateral femoral compartment were in good condition.
When the trochlea was removed, an examination of the patellofemoral compartment revealed Grade I arthritic alterations. The patella’s articular structure remained unchanged.
It was irrigated on the knee. 3-0 nylon was used for the closure. 40 mg of Depo Medrol and 9 cc of.5% Marcaine were injected into the knee. Dressing was carried out using ACE, 4 x 4, ABD, and Webril wrap. After being treated, the patient was transferred to the recovery area in stable condition.
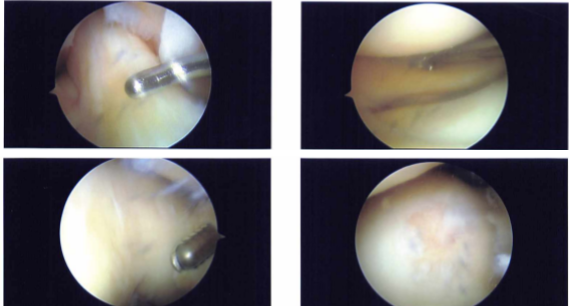
Intraoperative Images
After one week the patient is seen in the office for her post-operative consultation, her pain is well controlled, she denies fever or chills. After discussing treatment options, we have decided to proceed with formal physical therapy as well as a home exercise program for rehabilitation of the knee.
We went over the arthroscopic pictures and removed the stitches during the visit. We will continue with ice and elevation of the knee to decrease swelling and pain. We will continue to utilize early mobilization and mechanical prophylaxis to reduce the chances of a deep vein thrombosis.
We will wean them off any narcotic medications and progress to anti-inflammatories and Tylenol as long as there are no contraindications to these medications. We also discussed the risk and benefits and common side effects of taking these medications. The patient will be back in three weeks’ time to evaluate their progress.
After a month the patient is here today for her follow up checkup, the pain is well controlled. Denies fever and chills. She had been doing home PT and improving till 3 weeks post op when she started having pain in the outer knee and outer ankle right side. Her right hip pain is also worsening now.
She has started PT now. Another month has passed, the patient visits the office for her post operative consultation, her knee pain is well controlled, she has denied fever or chills but her both hip pain is worsening now. However, she has been working with her physical therapy and her knee pain has improved.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling. After a sterile prep, 7cc of 1% Lidocaine and 80mg of depo-medrol were injected into the right & left trochanteric bursa.
The patient tolerated the procedure well and there were no complications. Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail. The patient was instructed to contact us if there were any questions or concerns prior to their follow up appointment.
The patient did well after the surgery, from the time to time of his visits she is gradually improving. Through regular visits and continued physical therapy, the patient healed and recovered.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
