Case Study: Knee Arthroscopy: Medial Meniscectomy
and Abrasion Chondroplasty in a 61 year-old patient
For arthroscopic surgery to repair the meniscus, two to three small incisions must be made in the knee as opposed to one significant open incision. Through one of these incisions, your doctor inserts a tiny camera to give you a real-time view of the meniscus and the surgical procedure.
When the articular cartilage wears down and exposes the underlying bone, an abrasion chondroplasty is carried out. During this operation, the bone tissue from the joint’s surface is scraped off using a rotary burr.
Meniscus tears can cause persistent knee discomfort, a sense that your knee is giving way, and limitations on how you can move your knee. Osteoarthritis in the damaged knee may be more prone to occur.
A 61 year-old patient was in our office with complaints regarding bilateral knee pain from playing sports over many years. He had arthroscopic surgery on left knee which went well but the pain has recurred. For aggravating factors, patients reported standing, walking, and lifting.
For associated symptoms, he reports swelling but reports no weakness, no numbness, no tingling, no redness, no warmth, no ecchymosis, no catching/locking, no popping/clicking, no buckling, no grinding, no instability, no radiation, no drainage, no fever, no chills, no weight loss, no change in bowel/bladder habits, and no tenderness. For location, bilateral.
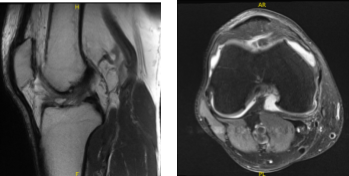
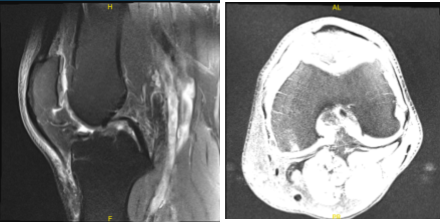
The patient presented MRI results for his left and right knees. For the right, moderate medial compartment arthrosis and a small horizontal tear along the superior articular surface of the posterior horn medial meniscus. There is evidence of previous partial medial meniscectomy.
There is mild lateral and patellofemoral arthrosis. There is a large joint effusion. For the left, Moderate-severe medial knee osteoarthritis with broad full-thickness cartilage loss and bone-on-bone apposition. Complex degeneration and tearing of the medial meniscus. Joint effusion with synovitis/debris.
MRI-3T Right knee non-contrast
MRI-3T Left knee non-contrast
We discussed treatment options and the patient opted for surgical management. We discussed the risks and benefits including infection, bleeding, injury to adjacent nerves and vessels, re-tear, need for repeat surgery, need for knee replacement in the future, and rehabilitation among others.
We discussed systemic complications including blood clot, cardiac, pulmonary, and neurology complications including death. The patient understood. We discussed the risks and benefits of doing both knees on the same day about staging them. The patient opted for both knees on the same day. Informed consent was taken.
The patient was taken to the operating room where he was put on a well-padded operating table. General anesthesia was induced. Both extremities were prepped and draped aseptically in the usual fashion. It was decided to do the left knee first as it was more symptomatic. Tourniquet was elevated.
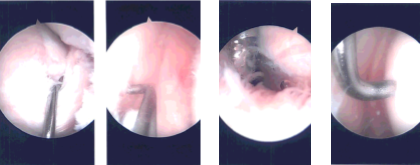
A left lateral entry portal was made through the and arthroscope was inserted. Medial entry portal was made with the use of spinal needle. Examination of the medial tibiofemoral compartment showed grade 4 osteoarthritic changes of the medial tibial plateau and grade 1 to grade 2 osteoarthritic changes of the medial femoral condyle.
It showed tearing of the medial meniscus in the region of the junction of the body and the posterior horn going into the posterior horn. Debridement of the medial meniscus was done with the use of shaver and biters. Debridement of the cartilage was also done with the use of shaver.
Abrasion chondroplasty of the tibial surface. Examination of the intercondylar notch showed degenerative ACL but not tear. Examination of the lateral tibiofemoral compartment showed no arthritis and no tear.
Examination of the patellofemoral compartment showed grade 2 to grade 3 osteoarthritic changes of the trochlea as well as patella. Debridement of the trochlea and patella was performed with the use of a shaver.
There was extensive synovitis in the suprapatellar region which was debrided with the use of shaver. Histopathology was sent for all the shavings. Final picture was taken and saved.
Intraoperative Arthroscopy Images
The knee was thoroughly irrigated and drained. Closure was done with the use of #3-0 nylon and dressing was applied. The tourniquet was released on the left side and elevated on the right side after application of Esmarch.
Similarly, a lateral entry portal was done on the right knee and an arthroscope was inserted. Medial portal was made with the use of a spinal needle. Examination of the medial tibiofemoral compartment showed grade 2 to grade 3 osteoarthritic changes of the medial tibial and femoral surfaces.
A tear of the medial meniscus along the junction of the body and the horn extending into the posterior horn was present. Debridement of the meniscus was done with the use of up-biters and shavers. Debridement of the cartilage was also performed.
Examination of the intercondylar notch showed degenerative ACL but no tear. Examination of the lateral tibiofemoral compartment showed no tear of the cartilage and no tear of the meniscus.
Examination of the patellofemoral compartment showed grade 2 to grade 3 osteoarthritic changes of the patella and trochlea which were debrided with the use of shaver. There was extensive synovitis in the suprapatellar region which was debrided with the use of shaver.
Histopathology was again sent of the right knee separately. The knee was thoroughly irrigated and drained. Closure was done with the use of # 3-0 nylon. Dressing was done with the use of 4x4s, Webril, and Ace wrap.
Xeroform was also applied as dressing on both knees. The patient was extubated and moved to recovery in a stable condition.
The patient was seen for post operative check up. We have decided to do formal physical therapy as well as a home exercise program for rehabilitation of the knee. Patients regularly followed an office visit every 3-4 weeks.
Patient did well after the surgery and continued physical therapy. Patient checked in for a follow up visit after a month and saw significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.