Case Study: Basic Operative Knee: Arthroscopic
partial Medial Meniscectomy and Chondroplasty
Knee pain is a common condition that impacts people of all ages and can be caused by an injury such as a ruptured ligament or torn cartilage. Knee discomfort can also be caused by medical conditions such as arthritis, gout, and infections.
Patient is a 43-year-old female, with complaints of right knee pain experiencing over a month. The patient remembers the injury to both knees in a car accident 3 years ago. The pain is moderate to severe in intensity. Patient describes the pain as dull, aching, stabbing. The pain is constant and does disturb sleep.
The pain is associated with swelling, clicking. The problem has been getting worse since it started. Walking, standing, lifting, exercise, twisting, bending, squatting, kneeling, and stairs make the symptoms worse. Rest, Heat, lying down makes the symptoms better.
Upon examination of the right knee, the patient is tender to palpation along the medial joint line, and has an effusion. There is pain along the medial and lateral PF joint line. The patient has discomfort with McMurray’s maneuvers, and the knee is stable.
They lack full flexion secondary to the effusion, but have full extension. They have 5/5 strength, and are neurovascularly intact distally. There is no erythema, warmth or skin lesions present.
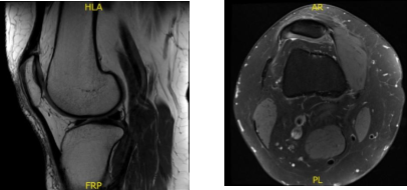
X-ray and MRI were presented in the office. Found vertical tear at the free edge margin of the posterior horn medial meniscus, with mild undersurface/free edge fraying of the body segment. Mild medial femorotibial compartment chondral loss. Mild patellofemoral compartment chondral wear, preferentially over the medial aspect of the compartment.
Lateral patellar tilt with mild lateral positioning of the patella. These findings may be seen in the setting of patellar malt racking. Features which may be seen in the setting of iliotibial band friction syndrome.

Lateral View
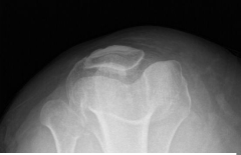
Patella Skyline

AP view
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits. The patient has expressed a desire to proceed with surgery.
We discussed treatment options and the patient opted for surgical management. We discussed the risks and benefits of surgery including bleeding. infection, knee stiffness, retear, need for repeat surgery, need for rehabilitation, no injury to adjacent nerves and vessels. The patient understood the risks, benefits, and complications well and signed an Informed consent.
General anesthesia was induced in the patient and the right lower extremity was prepped after application of tourniquet and Esmarch. The right lower extremity was draped aseptically.
A lateral entry portal incision was given. The arthroscope was introduced. The scope was moved to the medial tibiofemoral compartment where a medial entry portal was made using a spinal needle.
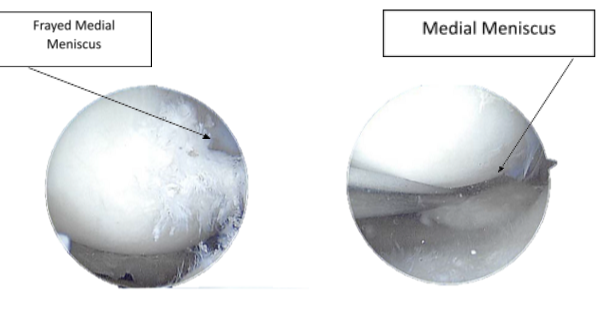
A probe was introduced. The medial meniscus tear was seen going through the body and the posterior horn up to the root. Shaver was introduced and the margins were cleaned. Upbiter and straight biter were used to remove the degenerated meniscus along the inside edge of the medial meniscus. The scope was moved to the intercondylar notch where an ACL was found to be intact with degeneration.
The scope was moved to the patellofemoral joint again where OA grade 3 to grade 4 lesion was found on the medial tibiofemoral condyle in the appropriate region. It was cleaned using an upbiter and shaver. The knee was reexamined and the medial meniscus was further debrided.
The chondral lesion of the medial femoral condyle was also shaved. The knee was copiously irrigated. The scope was removed. The incisions were closed using nylon #3-0. 20 cc of 0.5°/4 Marcaine was injected into the knee.
After a week of operation, a patient was seen in the office, she was walking with little discomfort. Denies fever, chills. Upon examination of the right knee reveals that there is a small effusion. The incisions are healing well, without evidence of drainage, erythema or warmth.
There is a limited range of motion secondary to discomfort. Strength distally is 5/5. There is no calf tenderness and a negative Homan’s sign. Sensation is intact to light touch distally and there is a brisk capillary refill.
After discussing the options for treatment and the risks of injection, the patient wished to proceed with the injection to reduce pain and swelling.
After a sterile prep, 3cc of 1% ropivacaine, 3cc of 0.5%marcaine and 80mg of depo-Medrol were injected into the right knee. The patient tolerated the procedure well and there were no complications.
Post injection pain, blood sugar elevation, skin discoloration, fatty atrophy and the signs of infection were discussed in detail. The patient returned to the clinic every 3-4 weeks. The patient recovered well from surgery and continued physical rehabilitation.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
