Case Study: Robotic Right Hip
Total Replacement in a 75-year-old male
A 75-year-old male presented to our office with complaints of right hip pain for the past 3 years. The patient didn’t recall the exact onset and any precipitating event leading to hip pain. The onset was insidious with gradual progression. He was recently in the emergency room for severe hip pain.
The pain was described as a dull ache that would progress to sharp pain on activity. The pain was located over the right groin, moderate in intensity with no radiation. Activities such as walking, sitting, bending, squatting and climbing stairs precipitated the pain. There was an associated stiffness especially after sitting for a prolonged period of time.
The patient was a retired police officer and felt his prolonged years of physical exertion at the job caused his hip pain. He was now living with his wife and daughter. He ran a small hardware store and remained physically active.
Secondary to pain, he seldom went to his store and had restricted his activities. He felt stressed out being not active and his wife was equally worried. He had previously tried hip injections, physical therapy, and heat pads but with minimal relief. His past surgical history included a right knee replacement done 8 years ago by an outside physician.
The patient was a nonsmoker, nondrinker and had no known drug allergies. His medical history included diabetes mellitus, hypertension, and dyslipidemia all well controlled with medications. He was currently on Januvia, Norvasc, and Lipitor. He was using a cane for ambulatory aid.
His physical examination revealed a steady but antalgic gait with reduced stance phase on the right side. There was no evidence of exaggerated lumbar lordosis and scoliosis. Both the shoulders, iliac spines were at the same level. There was no atrophy of the buttocks and thighs.
The skin overlying the right groin was normal with no scar, sinus or erythema. There was no fullness in the Scarpa’s triangle and no enlarged inguinal lymph nodes. The range of motion of the right hip was restricted terminally due to pain. There was no fixed sagittal or coronal plane deformity. Both the internal and external rotation of the right hip was painful.
There was tenderness at the right anterior hip joint line. There was no thickening or broadening of the trochanters. There was no leg length discrepancy and both the trochanters were at the same level on digital palpation. The examination of the left hip, bilateral knees and ankles were normal.
There was no distal neurological deficit. The distal extremity pulses were good volume and palpable. There was a linear scar over the right knee consistent with a previous right knee replacement. Imaging studies revealed severe osteoarthritis of the right hip.
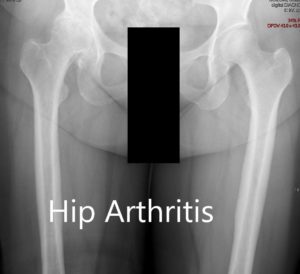
Preoperative X-ray showing the AP view of the pelvis with both hip joints.
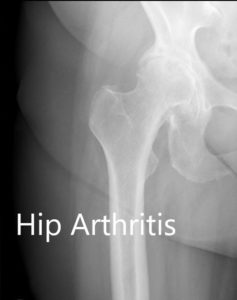

Preoperative X-ray showing the AP and the frog-legged lateral view of the right hip
After careful consideration of the patients’ comorbidities, he was advised a robotic right hip replacement. Risks, benefits, and alternatives were discussed with the patient at length. The patient agreed to go ahead with the procedure. The patient was assessed and medically cleared for the procedure.
OPERATION: Robotic right hip replacement.
IMPLANTS USED: Tritanium shell 48-mm with a high walled polyethylene liner, 127 degrees high offset stem with ceramic femoral head 32 mm+4
DESCRIPTION OF PROCEDURE: The patient was brought to the operating room after obtaining the informed consent, anesthesia was then obtained by the anesthesiologist. The patient was definitely positioned with the right hip up and the right hip was then prepped and draped in the usual sterile manner.
The skin incision was then made and the skin and subcutaneous tissues were then incised. The fascia was then divided. The hip was then placed into internal rotation and the posterior soft tissue structures were taken down and tagged for future repair. The hip was then dislocated after marking the femur with the robotic system.
The neck resection was then performed. Attention was then turned towards the femur. Additional bone morphing was done with the robotic system and the acetabulum was then reamed and the final cup was then placed into position using the robotic system. The head was then placed over the cup after placing a screw for additional fixation.
Attention was then turned towards the femur. The femur was then sequentially broached. The final broach was left into position and the trunnion and head were then placed into position. The hip was then reduced. The limb lengths were then compared to the preoperative planning and the limb lengths were found to be accurate.
The hip was then dislocated. Trial components were then removed. Sterile lavage was given. The final components were then placed into position. Limb lengths were then compared again based on the preoperative planning.
Pins of the robotic system were then removed and the hip was trialed through a range of motion and stability and was found to be acceptable.
Thorough lavage was given. The posterior soft tissue checks were then repaired. The fascia was closed with Ethibond. Cutaneous tissue was closed with 0-Vicryl. Subcutaneous tissue was closed with 2-0 Vicryl.
The incisions over the iliac crest for the pins were closed with 2-0 Vicryl and staples. Sterile dressing was then applied over the wound and the patient was returned to the postoperative care in stable condition.
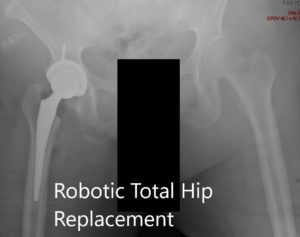
Postoperative images showing the AP and lateral images.
The patient has an excellent recovery postoperative. He was started on a combination of oxycodone and acetaminophen for pain. Aspirin 325 mg BID was started for deep vein thrombosis prophylaxis. The patient was discharged the subsequent day with hip precautions. He was allowed weight bearing as tolerated.
The sutures were inspected to be clean, dry and intact. They were removed 12 days postoperative. The patient was walking without support after a month. He was following up with outpatient physical therapy focusing on a range of motion and muscle strengthening. The patient was happily back to his hardware store with gait training. He follows up as needed.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
