Case Study: ACL reconstruction using
Quadriceps Tendon Autograft in a 38 yr old female
The patient was a 38-year-old female who was seen by me in the office with complaints of pain and instability of the right knee. He stated that he was hit by a pick up truck from behind, following which she was able to do all usual activities including running without pain before the accident in 2021.
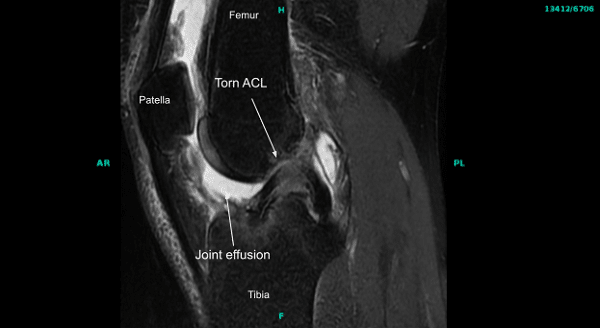
Physical examination was positive for ACL deficiency in the right knee. MRIs of the right knee joint confirmed the injury to ACL. No other pathology was seen. The patient had tried physical therapy in the past with no benefit.
We discussed the treatment options for the patient’s diagnosis, which included: living with the extremity as it is, organized exercises, medicines, injections and surgical options. We also discussed the nature and purpose of the treatment options along with the expected risks and benefits.
The patient has expressed a desire to proceed with surgery, and we think that is a reasonable option. The patient was educated on the inherent and unavoidable risks which include, but are not limited to: infection, stiffness, damage to nerves and blood vessels, blood loss possibly requiring transfusion, blood clots, persistent or worsening pain, loosening or failure of implants, instability, tingling or numbness, anesthesia and systemic complications including cardiac, pulmonary, neurological complications and even death were discussed at length.
We also talked about the possibility of not being able to return to prior activities or employment, the need for future surgery, and complex regional pain syndrome. The patient also understood there is a long rehabilitative process that typically follows the surgical procedure.
We talked about the possibility of not being able to alleviate all the discomfort and we also explained there is no guarantee all the function and strength will return. We discussed the type of implants that may be utilized during this surgery. The patient expressed understanding of these risks and has elected to proceed with surgery.
We discussed the patient’s medications and allergies and the possible need for medical and other clearances if needed. Ample time was given for questions, of which many were addressed. We have discussed the surgical procedure as well as the realistic expectations regarding the risks, outcome and post operative protocol. He was planned for ACL reconstruction with Quadriceps autograft electively.
The patient was taken to the operating room and placed on a well-padded operating room table. Local block was given by the anesthesiologist. General anesthesia was given and the patient was intubated.
The right lower extremity was prepped and draped aseptically in the usual fashion after application of the tourniquet. Preoperative antibiotics were given. The tourniquet was elevated after Esmarch. Examination under anesthesia showed ACL laxity with a soft ending collaborating with the MRI finding of absent ACL..
An incision was made over the proximal pole of the patella into the quadriceps. It was about a 2 cm incision. With deep dissection the region of the quadriceps was released. The paratenon was cut in the line of incision. The paratenon was stripped from the quadratus tendon proximally up to about 10 cm and distally onto the patella.
With the retraction the tendon could be seen. A linear flap was found on the skin for gutting the quadriceps tendon. 10 mL was used to cut a 10 mm quadriceps tendon right from the tip of the superior pole of the patella into the quadriceps tendon just lateral to the vastus medialis.
With the use of a knife the quadriceps tendon, which was cut, was elevated from the proximal volar patella. Full thickness quadriceps bone graft was elevated with the use of sharp dissection. This was followed by insertion of the cigar cutter so as to extract the graft. About 68 mm of quadriceps tendon was cut and put on the back table.
The capsule of the knee joint was not reached in the process. The quadriceps tendon was prepped with the use of FiberLink on either side and tight ropes. A lateral anterior portal was made with a lateral parapatellar incision and the arthroscope was inserted.
Examination of the patellofemoral compartment showed intact cartilage. Examination of the medial patellofemoral compartment showed intact meniscus and cartilage. Examination of the anterior condyle notch showed absent ACL from the proximal attachment.
Examination of the lateral tibiofemoral compartment showed intact cartilage with degenerative tearing and through the edge of the lateral meniscus with no debridement being done, as the meniscus was intact.
Debridement of the intercondylar notch was done to remove the ACL stump and to prepare the medial surface of the lateral femoral condyle at the intercondylar region tor the bone graft. Shaver followed by a Coblation wand was used in the process of preparation.
The quadriceps tendon was repaired and the 9.5 mm quadriceps gaff was achieved. FiberLinks were applied on either side. Measurements were done and it was marked at 55 mm on each side.
Now the ACL femoral was entered through the lateral portal and it was placed on the medial surface of the lateral femoral compartment, medial femoral condyle. An incision was made over the lateral femoral condyle and sleeve was inserted with the zig in appropriate position at 10:30 position, with about 7 mm from the posterior condylar edge.
The sleeve was pushed to the bone followed by insertion of a flip cutter. The flip cutter was drilled into the lateral femoral condyle and was seen through the medial surface. Finding it in the appropriate position the sleeve was impacted into the bone and the flip cutter was flipped to 9.5 mm and a 30 mm tendon was split into the femoral condyle.
The flip cutter was again pushed back into the knee joint and closed and achieved out followed by insertion of a fiber loop which was extracted and logged onto itself. Now the arthroscope was inserted from the lateral anterior portal and a tibial tunnel was planned. A 10 mm tibial lig was inserted and put posterior to the inter meniscus ligament just medial to the medial tibia.
A separate skin incision was given followed by insertion of a sleeve. Flip cutter was again inserted and drilled to make a tibial tunnel. Finding it in the appropriate position the sleeve was impacted again onto the bone and the flip cutter was flipped to 9.5 mm and a 30 mm tunnel was made.
The flip cutter was removed and the tibial tunnel was encapsulated with the use of Fiber Loop locked onto itself. The Fiber Loops were retrieved from the lateral portals and the medial portal site was then pieced appropriately for the passage of the tendon. Now the tibial loop was opened up and the graft was loaded on the femoral loop and inserted under visualization from the arthroscope from the lateral portal. The sutures were seen passing followed by passing of the button which was flipped on the lateral femoral cortex.
Now the tightrope was used to pull the tendon in. About 25 mm of tendon was pulled into the tunnel. At this time, the side of the graft was loaded onto the tibial fiber loop and passed into the tibial tunnel about 20 mm of graft could be passed on the tibial side.
Again the button was flipped onto the tibial cortex and it was toggled to tighten the graft. The graft was found to be in an appropriate position. The knee was cycled thirty times and the final tightening of the tight ropes were done on either side.
Examination of the graft showed acceptable alignment. The sutures were cut under the skin. The knee was thoroughly irrigated and then final pictures were saved. Closure of the wounds were done using 2-0 Vicryl and 3-0 Monocryl. Dressing was done with the use of Dermabond, Steri-Strips, 4×4 sterile gauze, Webril and ACE wrap, A knee immobilizer was applied.
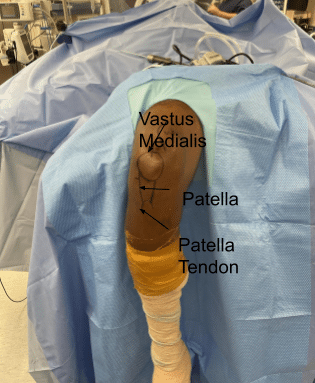
Actual footage of the operation
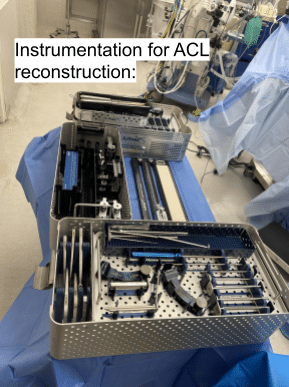
Instrumentation of ACL reconstruction
The patient was extubated and moved to the recovery room in stable condition. The patient was followed regularly as an outpatient in the office. Physical therapy was started and it helped in recovery of the patient. She went on to have an uneventful recovery. She was back to work in about 3 months and continued PT and made recovery in the next 8 months.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
