Case Study: Right shoulder Rotator Cuff Repair, Acromioplasty
Distal Clavicle Excision and biceps tenodesis
Patient is 43 years of age and here with complaints of right shoulder pain that he states started two years ago when he fell. He states this happened at work two years ago but is not a workers compensation case. He has tried PT and cortisone injection in left shoulder with temporary relief.
He also had radiating pain and tingling in right hand with neck tilted to the right side. We agreed to go with 3 tesla MRI of the right shoulder, considering that the last MRI is old and the patient still has pain.
MRI showed an impression as follows: High-grade partial-thickness articular sided tear of the infraspinatus tendon. Moderate supraspinatus tendinosis. Mild long head biceps tendinosis. Mild AC arthrosis. Moderate degenerative tearing of the superior labrum. We discussed treatment options and the patient opted for surgical management.
The patient was brought to the operating room where we discussed risks and benefits and complications of surgery including infection, bleeding, nonhealing, need for repeat surgery, shoulder pain, adhesive capsulitis, need for rehabilitation, injury to nerves and vessels among others.
We also discussed systemic complications. The patient understands and signed Informed consent.
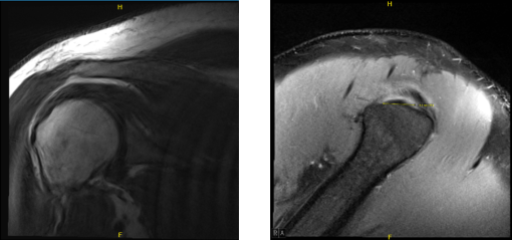
MRI of right shoulder
The patient was taken to the operating room where he was placed on a well-padded operating table. General anesthesia was induced. Preop antibiotic was given. The patient was turned in the left lateral position with the right shoulder up. The patient’s position was held in a beanbag.
The patient was tilted 45 degrees towards the bed. The right upper extremity was preppe d and draped aseptically in the usual fashion. The right upper extremity was put in traction at 45 degrees of abduction and flexion with 10 pound weight. Time-out was called.
A posterior anterior portal was made in the soft spot. An arthroscope was entered into the shoulder joint and examination was done. Entry on the lateral portal was made using a spinal needle. There was labral degeneration, which was debrided with shavers.
There was a tear of the rotator cuff on the articular side. This was debrided. The tear was found to be high grade with loss of almost 0.8 to 1 cm of rotator cuff footprint. There was degenerative partial tearing of the subscapularis, which was also debrided. There was no osteochondral damage on the glenohumeral joint. PDS was used to tag the area of the rotator cuff tear.
After the pictures were taken from the glenohumeral joint, the arthroscope was entered in the subacromial space. The subacromial bursitis was present, which was debrided using a shaver. The PDS was located and the rotator cuff was found to be thin in that area. The tear was completed using the shaver.
Subchondroplasty was done using Coblation wand and burr. Footprint for the repair of the rotator cuff was prepared and a 4-tail HEALICOIL Smith and Nephew anchor was inserted after tapping was passed through the anterior and posterior end of the rotator cuff tendon and tied on to each other. was also performed to supplement the repair.
AC joint was found to be having arthritis and hypertrophy. Distal clavicular excision was done using Coblation wand and burr. About a cm of clavicle was removed. Final pictures were taken and saved. The wound was thoroughly irrigated and drained. Closure was done.
On examination of the acromioclavicular joint, biceps inflammation was found, but there was no tearing. The biceps anchor was in a good position. It was decided not to do a biceps tenotomy or tenodesis.
The shoulder joint was irrigated and drained. Closure was done using #3-0 nylon. Dressing was done using Adaptic, 4×4, ABD. Shoulder immobilizer was applied. The patient was extubated and moved to recovery in a stable condition.
Patient returned to our office after a week of post-operative, no x-rays were needed. No fever, chills and the pain is well controlled. Post Operative Exam: General Appearance: no swelling, tenderness, or warmth and wound clean and dry, appropriate range of motion, and neurovascular intact.
The patient tolerated the procedure well and there were no complications. Post aspiration pain, and the signs of infection were discussed in detail. Patient checked in for follow up visit after a month and seen significant improvement on his knee.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
