Case Study: Shoulder Arthroscopy with Rotator Cuff Repair
using Labral Tape and Suture anchor in a 29 year-old girl
The technical parts of rotator cuff restoration include the insertion of tiny screws into the top region of the arm bone (humerus), where the rotator cuff tendon normally attaches. Suture anchors are screws composed of a unique type of biodegradable plastic that the body will naturally absorb over time.
Suture anchors are utilized to restore the rotator cuff tissue to the bone after it has been ripped. The surgeon will normally use three rotator cuff anchors or, in rare cases of major supraspinatus tendon rips, four rotator cuff anchors to stabilize the supraspinatus tendon.
The patient is a 29-year-old girl who came to see me after being involved in a car accident and complaining of an anterior shoulder ache on the left side. Physical therapy and anti-inflammatory medicines were ineffective. We performed an MRI, which revealed a type 2 labral tear.
We examined treatment alternatives and decided on surgical intervention. We reviewed the dangers and benefits of injection, hemorrhage, nerve and vascular injury, the necessity for repeat surgery, and the need for rehabilitation, among other things.
We talked about systemic concerns such as blood clots and cardiac, pulmonary, and neurological issues. The informed consent was understood and signed by the patient.
The patient was brought to the operating room and placed on a well-padded operating table. The anesthesia department administered a supraclavicular block before surgery. The patient was anesthetized, placed in the right lateral position, and supported by a bean bag.
All of the bony prominences were adequately cushioned. An axillary roll was installed. She was securely fastened to the bed. As usual, the left shoulder was prepared and draped aseptically.
With a 10-pound weight in traction, the arm was placed in 40-degree abduction and flexion. A timeout was issued. A preoperative antibiotic was administered.
The soft area was incised posteriorly, and the arthroscope was introduced into the glenohumeral joint. A labral tear around the front labrum was discovered during a glenohumeral joint examination. The biceps anchor and tendon were excellent.
A spinal needle was used to create an anterior inferior portal right above the subscapularis muscle. For additional investigation, a cannula was implanted. Further inspection revealed no evidence of cartilage loss.
There was no tear in the rotator cuff. The posterior inferior labrum was completely intact. The biceps anchor was still in place. The choice was made to repair the labrum.
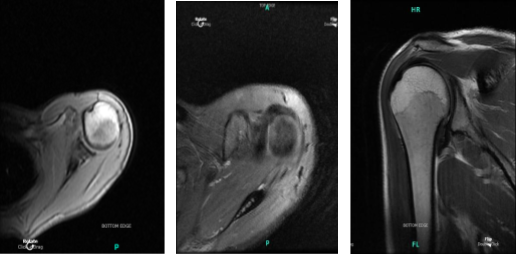
MRI Left shoulder non-contrast
Using spinal needles, an anterior superior entrance hole was created. Cannulas were swapped. To prepare for labral repair, the anterior glenoid was cleansed and grabbed with a shaver. A suture lash was inserted into the anterior labrum and replaced with labral tape.
The labral tape was inserted into the front glenoid using a pre-tapped bone anchor. The bone anchor had become flush with the bone. The extra suture was removed with a tape cutter. Pictures were captured and stored once more. After the repair, the labrum was stable.
The glenohumeral joint was irrigated and drained carefully. The arthroscope was introduced into the subacromial area, where there was no rotator cuff rupture or impingement and no normal bursa.
The arthroscope was removed, and the shoulder was irrigated and drained thoroughly. Photos were saved. Closure was accomplished with 3-0 nylon. In stable condition, the patient was placed in a shoulder sling and sent to recovery.
After one week the patient was seen in the office for her postoperative visit, no x-rays needed, her pain has improved but not resolved because she has a very low threshold for pain. We chose to proceed with a home workout regimen for shoulder rehabilitation after discussing therapy choices.
During the visit, we removed the stitches. We will continue to use ice and elevate the shoulder to reduce swelling and pain. We will gradually wean them off any narcotic medications and transition them to anti-inflammatories and Tylenol as long as there are no contraindications.
We also covered the risks and benefits of taking these medications, as well as the most prevalent side effects. The patient will return in three weeks to assess their progress.
The patient visits the office for her one month post operative consultation, no x-rays needed. Her pain has improved but not resolved. However, she is comfortable and looking forward to weaning off the sling. We decided to use cautious management for the time being. PT will start.
To lessen discomfort and swelling, we will still utilize ice and elevation, and we will keep taking over-the-counter anti-inflammatory medications. His follow-up 4 weeks later.
After two months of the patient seen by the doctor, the pain has improved but not resolved. She is comfortable now and is not using a sling. Aside from the pain is controlled and has no fever or chills.
She is improving gradually with PT. The patient’s progress and development have been undeniable with continued physical treatment and regular attendance at his follow-up checkups.
Disclaimer – Patient’s name, age, sex, dates, events have been changed or modified to protect patient privacy.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
